4835
MRI based measurement of pancreas motion reduction with an MR- and particle therapy compatible abdominal corset1Oncoray – National Center for Radiation Research in Oncology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Helmholtz-Zentrum Dresden-Rossendorf, Dresden, Germany, 2Technische Universität Dresden, Carl Gustav Carus Faculty of Medicine, Dresden, Germany, 3Institute of Radiooncology-OncoRay, Helmholtz-Zentrum Dresden-Rossendorf, Dresden, Germany, 4Department of Radiotherapy and Radiation Oncology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany, 5National Center for Tumor Diseases (NCT), Partner Site Dresden, Germany, German Cancer Research Center (DKFZ), Heidelberg, Germany, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, and Helmholtz Association / Helmholtz-Zentrum Dresden-Rossendorf (HZDR), Dresden, Germany, 6German Cancer Consortium (DKTK), partner site Dresden, and German Cancer Research Center (DKFZ), Heidelberg, Germany
Synopsis
Particle beam therapy (PBT) is extremely sensitive to patient setup uncertainties and anatomical variations prior to and during dose delivery. Organ motion mitigation strategies are hence required to deliver the dose with high precision and accuracy. In this study, an MR- and PBT-compatible patient-individualized abdominal corset was developed and tested in 9 patients with abdominal cancer for its efficacy to reduce respiratory-induced motion. Pancreas motion was analyzed with and without corset by means of orthogonal 2D-cine and 4D-MRI.
Introduction
In particle beam therapy (PBT) respiratory-induced tumor motion is commonly accounted for by the definition of an internal target volume1 to cover the tumor in all respiratory phases. Consequentially, also a relatively large volume of healthy tissue surrounding the tumor is exposed to radiation. An appropriate immobilization of the target volume can improve the sparing of healthy tissues. Immobilization of target volumes located in the upper gastro-intestinal tract has been accomplished through abdominal compression bands or pressure plates. These, however, can exacerbate the proton beam range uncertainties when these devices extend into the treatment fields, thereby compromising an accurate dose delivery2. For this study, an MR- and PBT-compatible patient-individualized abdominal corset was developed to test its efficacy to reduce respiratory-induced pancreas motion as measured by means of orthogonal 2D-cine and 4D-MRI.Methods
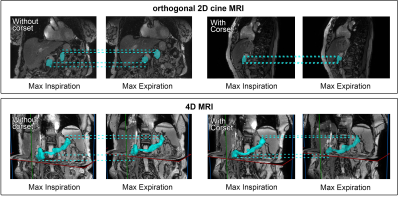
Nine patients (6 female, 3 male; average age 72.9 ± 9.6 years) with abdominal tumors of the pancreas (7 patients), gallbladder (1 patient), or liver (1 patient) provided written informed consent to be included in a clinical study (study number DRKS00010966) after study approval by the local Ethics Committee. Patients were scanned by means of orthogonal 2D-cine (2 min acquisition time) and 4D-MRI (9 min acquisition time) utilizing a balanced steady-state free precession sequence. For 2D-cine MRI coronal and sagittal slices were positioned at the pancreatic head. The 4D-MRI dataset was reconstructed by retrospectively resorting a multi-slice 2D acquisition into 10 respiratory phases by amplitude based sorting3, thereby imaging the full volume of the pancreas. Two MRI scans were acquired per patient, one without and one with a patient-individualized abdominal corset to reduce respiratory motion. The corset was manufactured from polyethylene (Orthopädie- und Rehatechnik Dresden GmbH, Dresden, Germany) based on an optical 3D-surface scan of the patient (Artec Eva®, Artec3D, Luxembourg, Luxemburg). From the nine patients, eight orthogonal 2D-cine datasets and seven 4D-MRI datasets were successfully acquired on a 3.0T MRI scanner (Ingenuity TF PET/MR scanner, Philips Healthcare, Best, The Netherlands). The patients were scanned in supine position on a flat tabletop using an anterior coil holder to avoid anatomical deformations of the chest wall due to the weight of the receiver coils. Pancreas motion was determined as center-of-mass displacement in three orthogonal directions (inferior-superior (IS), anterior-posterior (AP), left-right (LR)) for both orthogonal 2D-cine and 4D-MRI (Fig. 1). The motion amplitude extracted from the 2D-cine dataset was evaluated as the mean peak-to-peak amplitude M95, for which the lower and upper 2.5 % of the data was discarded to reduce the effect of possible outliers.Results
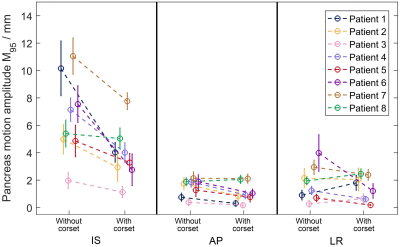
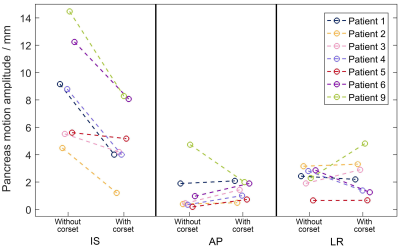
Orthogonal 2D-cine MRI showed that pancreas motion was dominant in IS direction (Fig. 2). For the 8 patients analyzed, the abdominal corset reduced the motion M95 in IS direction by in average 42 % (5 mm ± 3.7 mm (standard deviation) without corset, 3.8 mm ± 1.1 mm with corset; p<0.05). Similarly, the patients’ intrafraction motion variability decreased by 40 % (from in average 1.5 mm ± 0.4 mm to 0.9 mm ± 0.2 mm, p<0.01). Pancreas motion in AP and LR direction was small without corset (1.5 mm ± 0.2 mm and 1.8 mm ± 0.7 mm for AP and LR, respectively) and was not significantly reduced by the use of the corset (Fig. 2). In general, 4D-MRI (Fig. 3) showed larger motion amplitudes than 2D-cine MRI. For the 7 patients analyzed based on 4D-MRI, mean peak-to-peak motion in IS direction was reduced from 8.6 mm ± 3.7 mm without corset to 5.0 mm ± 2.4 mm with corset (42 % reduction, p<0.05).Discussion
Both orthogonal 2D-cine and 4D-MRI show that by use of a patient-individualized abdominal corset, respiratory-induced pancreas motion as well as the patient’s intrafraction motion variability can be significantly reduced in IS direction. The slightly different results retrieved with 2D-cine and 4D-MRI can be attributed to the different volume of the pancreas imaged in the respective modality. However, the main effect explaining this difference seems to be the amplitude-based sorting algorithm used for 4D-MRI, which naturally reflects larger motion amplitudes.Conclusion
MRI-based motion analysis showed that respiratory-induced pancreas motion could be significantly reduced in IS direction by the use of a patient-individualized MR- and PTB-compatible abdominal corset. The results suggest that patients would benefit from a patient-individualized abdominal corset allowing for improved healthy tissue sparing due to the consequentially smaller margins surrounding the target volume.Acknowledgements
No acknowledgement found.References
1 Chang JY, Zhang X, Knopf A et al. Consensus Guidelines for Implementing Pencil-Beam Scanning Proton Therapy for Thoracic Malignancies on Behalf of the PTCOG Thoracic and Lymphoma Subcommittee. Int J Radiat Oncol Biol Phys 2017; 99(1): 41-50.
2 Wroe AJ, Bush DA and Slater JD. Immobilization Considerations for Proton Radiation Therapy. Technol Cancer Res Treat 2014; 13: 217–226.
3 Von Siebenthal K, Székely G, Gamper U, Boesiger P, Lomax A and Cattin P. 4D MR imaging of respiratory organ motion its variability. Phys Med Biol 2007; 52: 1547–64.
Figures