4831
Does the timing of immunotherapy with stereotactic radiosurgery affect the outcome of patients with brain metastases?1Oslo University Hospital, Oslo, Norway, 2Hospital of Southern Norway, Kristiansand, Norway, 3Østfold Hospital Trust, Kalnes, Norway
Synopsis
The introduction of immunotherapy (IMTx) has led to a paradigm shift in the treatment of patients with metastatic cancer. Particular interest has been directed towards combining IMTx with stereotactic radiosurgery (SRS) to improve treatment response. Lately, studies have indicated that the timing of IMTx with SRS may be crucial for the patient outcome, suggesting that there is a window of opportunity to induce an optimal synergy between irradiation and immune agents. To this end, this work investigates whether the timing of IMTx with SRS affects the outcome of patients with brain metastases.
INTRUDUCTION
Attributed in large by advances in treatment of primary tumors over the last decades, there has been a substantial increase in cancer patients developing metastatic disease. For patients developing brain metastasis, the prognoses are often dismal with an overall survival from first diagnosis ranging from months up to a few years. Although advances in treatment strategies have been beneficial in terms of prolonged survival, the success often comes at the cost of clinical and neurological deficits. Hence, patients with brain metastases represent an increasing demand on health care resources, especially for repeated therapeutic interventions and diagnostic work-up. The introduction of immunotherapy (IMTx) has led to a paradigm shift in the treatment of patients with metastatic cancer, in which the power and specificity of the immune system is harnessed to treat the disease. Particular interest has been directed towards combining IMTx with stereotactic radiosurgery (SRS) to improve treatment response. Lately, studies have indicated that the timing of IMTx with SRS may be crucial for the patient outcome, suggesting that there is a window of opportunity to induce an optimal synergy between irradiation and immune agents1,2. The purpose of this study was to investigate whether the timing of IMTx with SRS affects the outcome of patients with brain metastases. Moreover, by using advanced magnetic resonance imaging (MRI), this study also explores different hemodynamic parameters that may provide a better understanding into the response mechanisms following IMTx and SRS.MATERIALS AND METHODS
Seventy-four patients from an on-going observational imaging study (TREATMENT study; clinicaltrials.govidentifier: NCT03458455) with brain metastases from primary non-small cell lung cancer and malignant melanoma were included in this interim analysis. Advanced study-MRIs, including dynamic susceptibility contrast (DSC) MRI, were performed pre-SRS and longitudinally for up to 36 months. All patients received SRS (15-27Gy) to on average 1.9 metastases within one week of the pre-SRS MRI. The patients were classified into three treatment groups: 1) SRS only, 2), non-concurrent SRS and IMTx, and 3), concurrent SRS and IMTx (±4 weeks). The immunotherapy included anti-PD-1 (pembrolizumab, nivolimumab or atezolizumab) or anti-CTLA-4 (ipilimumab), or a combination of the two. Patient demographics are shown in Table 1. Overall survival was assessed from the time of the pre-SRS MRI using Kaplan-Meier plot. Patients in group 2 and 3 were further investigated by estimating hemodynamic parameters from MRI data acquired at baseline and the 3 months follow-up. Voxel-wise estimations of the cerebral blood flow (CBV), cerebral blood volume (CBV), and mean transit time (MTT) were acquired using an established tracer kinetic model for DSC-MRI. All parameters were normalized to corresponding values in the grey and white matter. Furthermore, regions of interest (tumor tissue/contrast enhancing tumor tissue) were identified on high spatial resolution post-contrast MRIs and co-registered to the functional MR images. The Wilcoxon rank sum test was used to compare the hemodynamic parameters estimated in Group 2 and 3.RESULTS
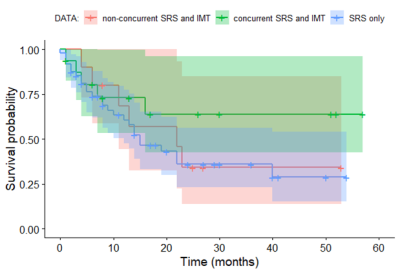
Our preliminary findings indicate that study patients receiving concurrent SRS and IMTx depict a clear trend towards improved overall survival compared to patient treated with SRS only or non-concurrent SRS and IMTx (Fig. 1). However, while still underpowered, the differences found in our interim analyses were not statistically significant (Group 1 vs. Group 3; P-value= 0.14 and Group 2 vs. Group 3; P-value= 0.74). At the 3 month follow-up, patients that had received concurrent SRS and IMTx showed a significantly higher MTT (P = 0.03) compared to patients receiving a non-concurrent treatment regime (Fig. 2), as well as a trend towards higher CBV (P = 0.08) and CBF (P = 0.11). Note that there was no significant difference in MTT between these two groups at baseline. Figure 3 show an example case of the normalized MTT parametric map overlaid a post-contrast 3D T1-weighted image at baseline and the 3 months follow-up.CONCLUSION
Our preliminary results indicate that combining SRS and IMTx may result in an improved survival in patients with brain metastases compared to SRS treatment alone, and that optimal treatment effect may be obtained if SRS and IMTx are given in a concurrent manner. This supports the hypothesis that there is a window of opportunity, thus the timing of IMTx with SRS may affect the outcome of patients with brain metastases. Our findings further indicate that the hemodynamic parameter MTT may be of importance as a means of understanding the therapeutic response mechanisms.Acknowledgements
No acknowledgement found.References
1. Brooks, E.D. and J.Y. Chang, Time to abandon single-site irradiation for inducing abscopal effects. Nat Rev Clin Oncol, 2019. 16(2): p. 123-135.
2. Reynders, K., et al., The abscopal effect of local radiotherapy: using immunotherapy to make a rare event clinically relevant. Cancer Treat Rev, 2015. 41(6): p. 503-10.
Figures