4830
Planning Reconstruction of Interstitial High Dose Rate Brachytherapy Needles based on MRI Data1Radiotherapy Physics, Mount Vernon Hospital, Northwood, United Kingdom, 2Paul Strickland Scanner Centre, Mount Vernon Hospital, Northwood, United Kingdom
Synopsis
Interstitial brachytherapy needles in High Dose Rate radiotherapy patients can be visualised clearly and accurately within clinical tolerance values using just a proton-density StarVIBE sequence instead of registered CT and MR images. This could lead to a reduced radiation dose MR-only workflow without compromising the quality of treatment and a reduction of errors in image registration.
Introduction
MRI is currently used with CT for HDR (High Dose Rate) brachytherapy treatment planning at this centre. Applicator reconstruction is performed on CT images, but OARs (Organs At Risk) and the CTV (Clinical Target Volume) are delineated primarily on MRI. We wish to image these patients solely using MRI, reducing uncertainties introduced when registering images, decreasing the ionising radiation dose received and improving the patient experience. However, in current practice, the interstitial needles cannot be visualised by MRI with enough accuracy (manifested as a high inter-operator variability in the reconstructed needle positions); therefore the focus of this project was to improve MRI needle visualisation.Background
The Varian plastic interstitial needles used (Varian Medical Systems, Palo Alto, USA) are hollow catheters inserted into the patient surgically prior to treatment and are where the radioactive source is inserted in order to give a radiation dose to the tumour. It is crucial that the needles can be reconstructed accurately in the Varian Eclipse™ Treatment Planning System (TPS) if an MR-only workflow is to be undertaken. It should be noted that because of the sharp dose fall-off in brachytherapy, CT electron density information is not required in the same way as for external beam radiotherapy planning.Initial work1 on visualisation and reproducibility agreed with our previous work2. Other centres have investigated this using contrast agents, for example Haack et al3. used CuSO4 while Otal et al. used vitamin-A marker points on the template4. Wang et al. used an MR tracking system which consisted of a stylet with micro-coils inserted into the catheter5. Zhou et al. also reported on successes at different centres using an electromagnetic tracking system6. There has been little success on the visualisation of brachytherapy applicators using sequence development alone.
Treatment planning for brachytherapy involves importing images into the TPS and then calculating the positions of the needles so sources can be placed optimally. This reconstruction needs to be done with images where the needles are easy to see. Sequences for MRI treatment planning at this centre are typically T2-weighted SPACE (TE 96ms, TR 1600ms, 1mm resolution) or T2-TSE (TE 99ms, TR 9930ms, 3mm resolution) which take 3-7 minutes. Patients are also prone to motion because of the surgery, so any sequence for identifying the needle positions needs to be fast, high resolution, and motion-insensitive with the needle artefacts being compact but prominent so positions can be assessed accurately, while flattening tissue contrast.
This led us to investigate a proton-density-weighted (PDW) radial volume-interpolated breath-hold excitation sequence (Star-VIBE; Siemens, Erlangen, Germany).
Methods
A combination of phantoms (Eurospin T1, in-house and fruit) was used to investigate the current imaging sequences (MRI and CT) and the proposed StarVIBE, with the aim of reducing signal variation in tissue so that the air cavities inside the needles could be clearly identified. Optimum flip angles and Signal to Noise ratios (SNR) were found. An in-house distortion phantom was used to compare reconstructed needle positions in the TPS on MRI and CT images.Following the phantom measurements and analyses, patients were imaged with the standard-of-care method and with the optimised StarVIBE to compare the sequences, under section 4.3.2.1 (testing sequences) of the MHRA Safety Guidelines7.
TPS positional errors were measured for three patients using all the imaging types and by eight operators, and inter-operator variability was assessed.
All work was conducted using a Siemens Aera 1.5T MRI, and a Siemens Definition planning CT.
Results
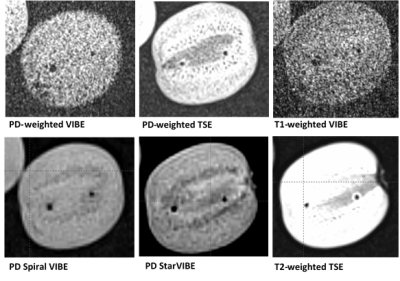
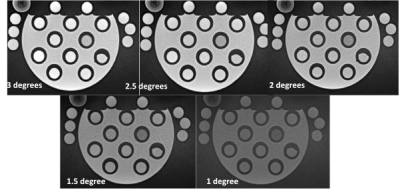
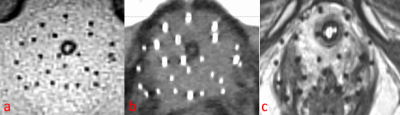
A comparison of image contrasts on a kiwi fruit is shown in Figure 1. The Eurospin T1 phantom StarVIBE images are shown in Figure 2. A PDW StarVIBE sequence using a 2o flip angle, slice thickness 1.3mm, TE 4.77ms and TR 6.8ms was considered optimum. This gave good air-to-tissue contrast and SNR, and was acquired radially in k-space, making it robust to motion artefacts. Initially, 520 out-of-phase radial views were used which led to artefacts at tissue boundaries. To eliminate these, subsequent data were acquired in-phase and using 320 radial views to minimise acquisition time. Figure 3 shows an optimised StarVIBE image and the corresponding CT for an HDR patient.The accuracy and variability analysis considered a total of 57 needles in 3 patients. The results of the inter-operator comparison on StarVIBE and CT images are summarised in Table 1. The overall mean difference seen using StarVIBE MR was 1.06mm, compared with 0.94mm when CT was used. Both are within the clinical tolerance of 2mm.
The results from the inter-operator study show similar inter-operator variability whether needles are visualised using the MR StarVIBE sequence or CT.
Discussion
Using MR-only avoids the uncertainty of the registration to CT, which could lead to an overall reduction in uncertainty. Furthermore, an improvement in operators’ ability to reconstruct applicators in the TPS using MR-only is expected when more experience is gained. There is potential to implement this method clinically. As this study has been conducted without MRI contrast or additional equipment this technique could be easily implemented by other centres. There is potential for a similar sequence to be used for MR-only I-125 seed low-dose-rate brachytherapy post-planning.Acknowledgements
No acknowledgement found.References
1. Newton V. et al., MR in the Radiotherapy Pathway, IPEM Meeting (2019) 2. Wills, R. et al., Applicator reconstruction for HDR cervix treatment planning using images from 0.35 T open MR scanner Radiother Oncol. 2010 Mar;94(3):346-52 3. Haack S. et al., Applicator reconstruction in MRI 3D image-based dose planning of brachytherapy for cervical cancer. Radiother Oncol. 2009 May;91(2):187-93. 4. Otal A. et al., A method to incorporate interstitial components into the TPS gynecologic rigid applicator library. J Contemp Brachytherapy. 2017 Feb;9(1):59-65 5. Wang W. et al., Evaluation of an active magnetic resonance tracking system for interstitial brachytherapy. Med Phys. 2015 Dec;42(12):7114-21 6. Zhou J. et al.,Review of advanced catheter technologies in radiation oncology brachytherapy procedures. Cancer Manag Res. 2015 Jul 16;7:199-211 7. Safety Guidelines for Magnetic Resonance Imaging Equipment in Clinical Use §4.3.2.1, MHRA 2015
Figures