4820
Prediction of therapeutic response of HCC to transcatheter arterial chemoembolization based on pretherapeutic dynamic enhanced MRI radiomics1The First Affiliated Hospital of Dalian Medical University, Dalian, China, 2Translational Medicine Team, GE Healthcare, Shanghai, China, 3GE Healthcare, Beijing, China
Synopsis
In the current study, dynamic enhanced MRI radiomics was demonstrated to be capable to predict therapeutic response in hepatocellular carcinoma treated with transcatheter arterial chemoembolization, which will provide more prognostic information and facilitate clinical management.
Purpose
To investigate the application of dynamic enhanced MRI radiomics to predict therapeutic response in hepatocellular carcinoma after transcatheter arterial chemoembolization (TACE).Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer and ranks as the fourth cause of cancer-related death worldwide[1]. TACE is a well established primary therapy for patients with unresectable HCC. It is widely accepted as a means to control tumor growth, to prolong survival in patients with unresectable HCCs, and to decrease the recurrence of resectable HCCs[2, 3]. Accurate assessment of therapeutic response to predict efficacy before the performance of TACE is important for treatment planning. Thus, it is necessary to explore an non-invasive method to preoperatively identify factors that can predict treatment response before TACE for guiding further surveillance and treatment. Radiomics is a rapidly growing field that converts medical images into high-dimensional quantitative features through different algorithms, potentially aidding in cancer detection, diagnosis, treatment response assessment, and prognosis prediction. Therefore, dynamic enhanced MRI radiomics was introduced in the present study to evaluate its clinical application performance in predicting therapeutic response of HCC after TACE.Materials and Methods
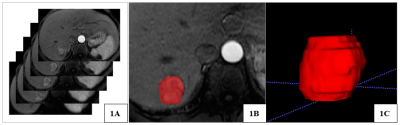
We retrospectively analyzed 61 HCCs treated with TACE who underwent dynamic enhanced MRI before initial TACE. The diagnostic criteria of HCC is confirmed by biopsy or in accordance with the latest guidelines of the American Association for the study of liver diseases (AASLD). All patients have underwent preoperative LAVA dynamic contrast enhanced MR examinations within 1 month before TACE and a follow-up MRI scan after TACE (with 4-8 weeks). To assess the tumor response, modified Response Evaluation Criteria in Solid Tumors (mRECIST) criteria was applied to MRI findings, and the mRECIST system grades target lesion responses as follows: complete response (CR), partial response (PR), stable disease (SD) and progressive disease (PD). We classified CR and PR as response treatment (RT) group, and SD and PD as non-response treatment (NRT) group. On the arterial phase MR images, two radiologists manually outlined the ROIs which enclosed the boundary of target lesions (shown in Figure 1) and extracted 792 radiomics features, which were composed of histogram features, formfactor features, texture (Haralick, GLSZM, GLCM, and RLM) features, and higher order statistics features via Gaussian transformation. Then, the general univariate analysis and least absolute shrinkage and selection operator (LASSO) algorithm were performed to identify the most predictive radiomics features. The multivariate logistic regression classifier was applied to build the radiomics model for predicting therapeutic response. Diagnostic performance was evaluated by receiver operating characteristic (ROC) analysis.Results
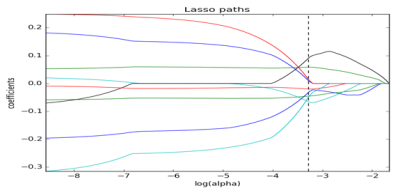
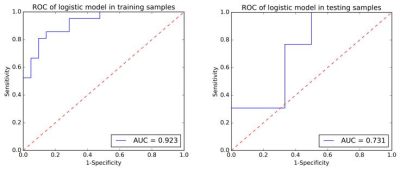
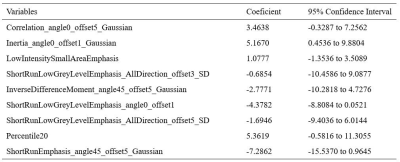
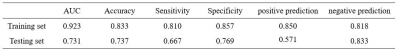
Figure2 showed the process of selecting the radiomics features by LASSO logistic regression model. Nine radiomics features were selected to build the radiomics signature using the LASSO logistic regression model (Table 1). The diagnostic performance and receiver operating curve (ROC) of the radiomics model were shown in Table 2 and Figure 3. In the training set, the AUC of the radiomics model was 0.923, an accuracy of 0.833, a sensitivity of 0.810 and a specificity of 0.857, respectively. In the testing set, the AUC of the radiomics model was 0.731, an accuracy of 0.737, a sensitivity of 0.667 and a specificity of 0.769, respectively.Discussion
The dynamic MRI radiomics based strategy has shown great potential in predicting therapeutic response of HCC treated with TACE. Discriminative features in the radiomics siganature are composed of specific categories: one histogram-based feature (Percentile20), three GLRLM-based features (three of ShortRunLowGrayLevelEmphasis), one GLSZM-based feature (LowIntensitySmallAreaEmphasis), and four higher order statistics features (Correlation, Inertia, InverseDifferenceMoment and ShortRunEmphasis). In the present study, arterial phase MR-based radiomics signature demonstrated satisfactory discriminative power both in the training and testing sets (AUC = 0.923 and 0.731, respectively).Conclusion
Dynamic enhanced MRI-based radiomics signature demonstrated good discriminative ability in predicting therapeutic response in hepatocellular carcinoma after performing TACE, which will provide more prognostic information and facilitate clinical managementAcknowledgements
No acknowledgement found.References
[1] Siegel RL, Miller KD, Jemal A. Cancer statistics 2016. CA Cancer J Clin. 2016; 66:7–30.
[2] Shim JH, Lee HC, Kim SO, et al. Which response criteria best help predict survival of patients with hepatocellular carcinoma following chemoembolization? A validation study of old and new models. Radiology. 2012; 262:708–718.
[3] Llovet JM, Real MI, Montana X, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002; 359: 1734–1739.
Figures