4801
High-temporal-resolution dynamic contrast enhanced MRI helps the diagnosis of the clinically significant lesions of prostate1Department of Diagnostic and Interventional Radiology, Shanghai Jiao Tong University Affiliated Sixt, shanghai, China, 2MR Application Development, Siemens Shenzhen magnetic Resonance Ltd, shenzhen, China
Synopsis
In clinical practice, definitions of the early enhancement are vague with different temporal resolution, and have caused some confusion. The aim of this study was to define the early enhancement in dynamic contrast enhanced (DCE)- MRI with high temporal resolution (5 sec), and to assess whether it can improve the detection of clinically significant lesions. The result indicated that the time to enhancement of clinically significant lesion was significantly different from those lesions with low grade or intermediate grade.
Purpose
DCE- MRI is primarily useful in the diagnosis of prostate lesions when diffusion weighted imaging is not definitive. Definitions of the early enhancement are vague with different temporal resolution, and have caused some confusion. The aim of this study was to define the early enhancement in DCE- MRI with high temporal resolution (5 sec), and to assess whether it can improve the detection of clinically significant lesions in the peripheral zone and transition zone.Materials and methods
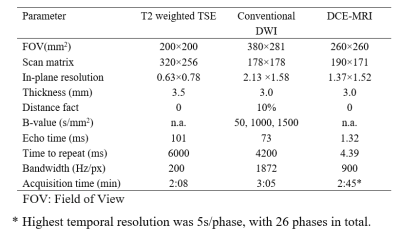
This prospective study was approved by the ethic committee of our hospital.From November 2018 to September 2019, consecutive patients with clinically suspected prostate cancer were enrolled. All patients underwent multi-parametric MRI of the prostate (including T2-weighted, diffusion-weighted imaging, and DCE-MRI using TWIST-VIBE technique with temporal resolution of 5 seconds) on a 3 T MRI scanner (MAGNETOM Skyra, Erlangen, Germany), Additional scan parameters are shown in Table 1. MRI fusion ultrasound biopsy was used as the reference standard. Semi-quantitative parameters of DCE, including TTE(time to enhancement), MS(maximum slope), TTP (time-to-peak), iAUC60(area under the curve within 60 sec after enhancement), PEI(relative peak enhancement), APEI(absolute peak enhancement),TTMS(time to center of max),WOS45(wash-out slope for 45 sec after peak) were calculated by using a prototype MR DCE software (Siemens Healthcare, Erlangen, Germany). The ability of the parameter to help differentiate tumors with a Gleason score of less than 6 (G6-) from those with a Gleason score of at least 7([Gleason score of 7, G7; Gleason score higher than 7, G7+]) was assessed by using the area under the receiver operating characteristic curve (Az).Results
Ninety-eight patients (69.8 ± 7.5 years) were enrolled in this study. For patients with multifocal lesions, the lesions with the largest sizes according to DWI were included. Thus a total of 98 lesions were analyzed in this study, including 7 lesions in the G6 group (GS = 6), 31 lesions in the G7 group (GS = 7), 20 lesions in the G7+ group (GS > 7), and 40 lesions with benign lesions. Of all included lesions, 50% originated in the peripheral zone; the others originated in the transition zone. Apart from TTE, no other parameter was significantly different between different groups. The TTE of the lesion in G7+ was significantly lower than that in G7 group (9.5±1.3 vs. 11.9±4.2 sec, P =0.046) and in G6- (9.5±1.3 vs.14.0±6.4 sec, P =0.038). However there was no significant difference of TTE between G7 and G6- group (11.9±4.2 vs. 14.0±6.4 sec, P =0.39). Using TTE as an independent predictor for differentiating lesions in G7 from those in G7+, the sensitivity, specificity, cutoff and AZ was 0.857, 0.444,11.0 sec and 0.762, respectively; when differentiating lesions in G7+ from those in G6-, the sensitivity, specificity, cutoff and AZ was 0.857, 0.423, 11.0 sec and 0.758 respectively.Conclusion
This study suggested that high temporal resolution of DCE could differentiate clinically significant lesions from those lesions with low grade or intermediate grade, which yields benefits when diffusion weighted imaging is not definitive. Larger number of lesions is warranted to confirm this finding.Acknowledgements
No acknowledgement found.References
1. Greer MD, Shih JH, Lay N, Barrett T, Kayat Bittencourt L, Borofsky S, Kabakus IM, Law YM, Marko J, Shebel H, Mertan FV, Merino MJ, Wood BJ, Pinto PA, Summers RM1, Choyke PL, Turkbey B. Validation of the Dominant Sequence Paradigm and Role of Dynamic Contrast-enhanced Imaging in PI-RADS Version 2. Radiology, 2017, 285(3):859-869.
2. Padhani AR, Weinreb J, Rosenkrantz AB, Villeirs G, Turkbey B, Barentsz J. Prostate Imaging-Reporting and Data System Steering Committee: PI-RADS v2 Status Update and Future Directions.Eur Urol. 2019,75(3):385-396.
3. Othman AE1, Fal.kner F, Weiss J, Kruck S, Grimm R, Martirosian P, Nikolaou K, Notohamiprodjo M. Effect of Temporal Resolution on Diagnostic Performance of Dynamic Contrast-Enhanced Magnetic Resonance Imaging of the Prostate.Invest Radiol. 2016, 51(5):290-296.
Figures