4786
Five-level scale for post treatment whole body MRI-DWI interpretation in lymphoma (Minsk scale): comparison with PET/CT Deauville scale1Radiology, N.N. Alexandrov National Cancer Center, Lesnoy, Minsk District, Belarus, 2PET/CT, N.N. Alexandrov National Cancer Center, Lesnoy, Minsk District, Belarus, 3Chemotherapy, N.N. Alexandrov National Cancer Center, Lesnoy, Minsk District, Belarus
Synopsis
PET/CT is a standard imaging technique for tumor response assessment in lymphoma. Deauville scale is used to interpret post treatment PET/CT studies. We proposed 5-level scale for whole body MRI-DWI exams interpretation (Minsk scale) in patients with lymphoma after treatment. Five-level structure of Minsk scale makes it comparable to Deauville scale. Treatment response assessment using MRI-DWI and Minsk scale match PET/CT results in 93 of 105 (89%) patients. Survival analysis confirmed prognostic value of Minsk scale. MRI-DWI and Minsk scale could be recommended for tumor response evaluation in lymphoma as non-irradiative alternative to PET/CT.
Introduction
Lymphomas are a group of malignant tumors of the lymphatic system that includes Hodgkin lymphoma (HL) and non-Hodgkin lymphomas (NHL). Lymph nodes (LN) and extralymphatic organs are affected by lymphomas. The main treatment method in lymphomas is chemotherapy. Positron emission tomography with 18-fludeoxyglucose combined with computed tomography (FDG PET/CT) is a recommended technique for tumor staging and treatment response evaluation in FDG-avid lymphomas while CT should be used in variably FDG-avid lymphoma subtypes.1 Five-level Deauville scale is used for post treatment PET/CT interpretation in lymphoma where assessment categories D 1-3 correspond to complete tumor response (CR) while categories D 4-5 correspond to non-complete response (NCR)2. Mediastinal blood pool and liver are used as reference tissues in Deauville scale. Effectiveness of whole body magnetic resonance imaging with diffusion weighted imaging (MRI-DWI) for lymphoma treatment response evaluation has been studded by several authors.3-8 MRI-DWI was interpreted visually or quantitatively using surround tissues, spinal cord or muscles as a reference tissues but not multiple levels interpretation scale analogous to Deauville one has been proposed till now. Such a scale will facilitate MRI-DWI interpretation allowing standardization and direct comparison with PET/CT. We aimed to develop MRI-DWI five-level scale for tumor response evaluation in lymphoma and to compare its effectiveness with PET/CT Deauville scale.Methods
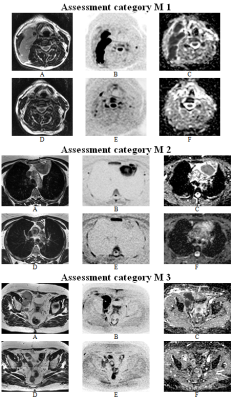
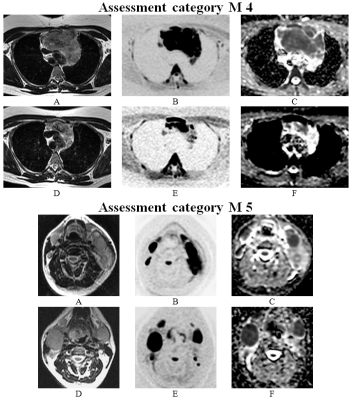
Local ethics committee permission was obtained for this prospective study. We included 105 adult lymphoma patients (age 43±15 y. o., males 56, HL 57, NHL 48) who underwent whole body MRI-DWI and PET/CT after the end of chemotherapy and were followed-up for at least 6 months. The number of chemotherapy courses ranged from 3 to 8 (median 6). MRI-DWI and PET/CT scanning was performed at the level from the base of skull to middle third of thighs with a median time between two exams of 7 days. MRI was performed with 1.5 T scanner equipped with built-in body coil. Coronal T1-weighted and STIR, transversal DWI and FIESTA images were obtained. Technical parameters for DWI were as the next: TR 4000 ms, TE 67 ms, TI 180 ms, b factor 0 and 800 s/mm2, slice thickness 5 mm, slice gap 1 mm, field of view 480×432, matrix 80×128, number of excitations 6. PET/CT was interpreted using 5-level Deauville scale. To interpret MRI-DWI, we developed 5-level scale named Minsk scale: M 1 – all LN decreased to normal size (< 1 cm in short axis), there are no extralymphatic lesions; M 2 – enlarged LN and lesions in the organs have signal intensity above the muscles on the apparent diffusion coefficient (ADC) maps, there is no bone marrow (BM) involvement; M 3 – enlarged LN and lesions in organs have signal intensity equal to muscles on ADC maps, there is no BM involvement; M 4 – enlarged LN and/or lesions in the organs have signal intensity below the muscles on ADC maps and/or there is a BM involvement; M 5 – an increase of lesions size and/or appearance of new ones (Fig. 1, 2). Assessment categories 1-3 were considered a sign of CR while categories 4-5 a sign of NCR for both methods. Biopsy or follow-up of minimum 6 months were used as a reference standard. Progression-free survival (PFS) and overall survival (OS) were compared between CR and NCR groups using Kaplan-Meier technique.Results
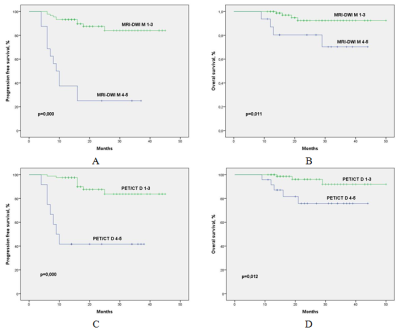
According to the reference standard, CR was established in 81 (77%) patients and NCR in 24 (23%). The following assessment categories were established with MRI-DWI: M 1 in 42 patients, M 2 in 23, M 3 in 24, M 4 in 12, and M 5 in 4 meaning CR was achieved in 89 (85%) patients. PET/CT assessment categories were as the next: D 1 in 35 patients, D 2 in 36, D 3 in 10, D 4 in 9, and D 5 in 15, that is CR was achieved in 81 (77%) patients. A complete match of MRI-DWI and PET/CT assessment categories occurred in 43 (41%) patients, and degree of tumor response (CR/NCR) matched in 93 (89%) patients. The agreement of MRI-DWI (κ=0.76, p=0.000) and PET/CT (κ=0.78, p=0.000) with the reference standard was good. The sensitivity, specificity, accuracy, positive and negative predictive value of MRI-DWI were 66.7%, 100.0%, 92.4%, 100.0%, 91.0%, PET/CT – 83.3%, 95.1%, 92.4%, 83.3%, 95.1%, respectively. The diagnostic effectiveness of the methods was not significantly different (ROC analysis, p=0.32). The most common reason for incorrect tumor response evaluation in MRI-DWI were non-enlarged LN, and in PET/CT – metabolically active non-tumor diseases. 3-year PFS with negative and positive MRI-DWI results was 93% and 25% (p=0.000), 3-year OS was 97% and 70% (p=0.011), respectively (Fig. 3).Conclusion
We proposed 5-level scale for interpretation of whole body MRI-DWI exams in patients with lymphoma after treatment – Minsk scale. Five-level structure of Minsk scale makes it comparable to Deauville scale used for PET/CT. Treatment response assessment using MRI-DWI and Minsk scale match PET/CT results in 89% of patients. Survival analysis confirmed prognostic value of Minsk scale. MRI-DWI and Minsk scale could be recommended for tumor response evaluation in lymphoma as an effective and non-irradiative alternative to PET/CT.Acknowledgements
No acknowledgement found.References
1. Cheson
BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation,
staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: The Lugano
Classification. J Clin Oncol. 2014;32(27):3059-3068.
2. Meignan
M, Itti E, Gallamini A, Younes A. FDG PET/CT imaging as a biomarker in
lymphoma. Eur J Nucl Med Mol Imaging. 2015;42:623-633.
3.
Kharuzhyk
S, Zhavrid E, Sachivko N. Diffusion-weighted MRI in the evaluation of
posttherapeutic residual masses in lymphoma. International Society for Magnetic
Resonance in Medicine 25th Annual Meeting & Exhibition: Proceedings,
Honolulu, 22-27 April 2017. – Honolulu, 2017. – 0869.
4.
Albano
D, Patti C, La Grutta L, et al. Comparison between whole-body MRI with
diffusion-weighted imaging and PET/CT in staging newly diagnosed FDG-avid
lymphomas. Eur J Radiol. 2016;85:313-318.
5.
Maggialetti
N, Ferrari C, Minoia C, et al. Role of WB-MR/DWIBS compared to (18)F-FDG PET/CT
in the therapy response assessment of lymphoma. Radiol Med. 2016;121:132-143.
6. Herrmann
K, Queiroz M, Huellner MW, et al. Diagnostic performance of FDG-PET/MRI and
WB-DW-MRI in the evaluation of lymphoma: a prospective comparison to standard
FDG-PET/CT. BMC Cancer. 2015;15:1002.
7. Mayerhoefer
ME, Karanikas G, Kletter K, et al. Evaluation of Diffusion-Weighted Magnetic
Resonance Imaging for Follow-up and Treatment Response Assessment of Lymphoma:
Results of an 18F-FDG-PET/CT-Controlled Prospective Study in 64 Patients. Clin
Cancer Res. 2015;21:2506-2513.
8. Littooij
AS, Kwee TC, de Keizer B, et al. Whole-body MRI-DWI for assessment of residual
disease after completion of therapy in lymphoma: A prospective multicenter
study. J Magn Reson Imaging. 2015;42:1646-165.
Figures