4774
Improved Prostate Cancer Detection: Comparison of Zoomed Diffusion- Weighted Imaging (DWI) with Conventional DWI1Department of Diagnostic and Interventional Radiology, Shanghai Jiao Tong University Affiliated Sixt, shanghai, China, 2MR Application Development, Siemens Shenzhen magnetic Resonance Ltd, shenzhen, China, 3MR Application Predevelopment, Siemens Healthcare, Erlangen, Germany
Synopsis
This study compared zoomed diffusion- weighted imaging (DWI) and conventional DWI of prostate lesions with respect to image quality, lesion detection capability, and diagnostic accuracy. The results demonstrate that zoomed DWI can provide improved image quality, including reduced artifacts and higher contrast-to-noise ratio (CNR), and aid in improved prostate cancer detection.
Background
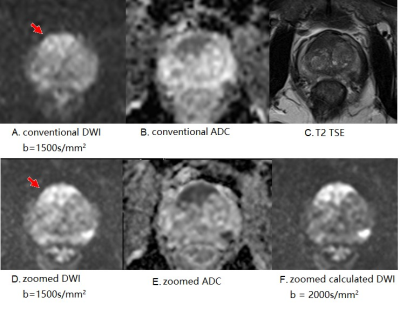
Diffusion-weighted images (DWI) of prostate acquired with single-shot echo-planar imaging (ss-EPI) sequences suffer from geometric distortion caused by the presence of rectum air or susceptibility artifacts relating to B0 inhomogeneity, which not only hampers the detection of prostate cancer foci but also influences the quantitative apparent diffusion coefficient (ADC) values. The zoomed EPI sequence, using a specially designed 2D excitation radiofrequency (RF) pulse which excites a much smaller field of view (FOV) to cover only the region of interest, can reduce distortion and susceptibility artifacts, as well as increase the spatial resolution and shorten the acquisition time of DWI [1-3]. The aim of this study was to compare zoomed DWI and conventional DWI for detection of prostate lesions with respect to image quality, lesion detection capability, and diagnostic accuracy.Methods
This prospective study was approved by the ethic committee of our hospital. From November 2018 to September 2019, patients with elevated prostate-specific antigen (PSA) underwent prostate MRI on a 3 T MRI scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany), including conventional DWI and a prototype zoomed DWI sequence utilizing a 2D RF pulse for excitation with b-values of 50, 1000, and 1500 s/mm2. Additional scan parameters are shown in Table 1. Calculated DWI images with b=2000 s/mm2 for zoomed DWI (zoomed calc- b2000) were derived from the acquired images using the mono-exponential decay model. The subsequent MRI fusion ultrasound biopsy was used as the reference standard. Image distortions and the presence of artifacts in both DWI sequences were rated on a 5-point scale by two readers independently. Lesion conspicuity based on the contrast-to-noise ratio (CNR) was compared for both techniques. The ability of the ADC derived from each the sequence to differentiate benign lesions from overall cancer [Gleason score (GS) ≥ 6)] or clinically important cancer (GS ≥ 7) was assessed by using the area under the curve (AUC) for the receiver operating characteristic curve.Results
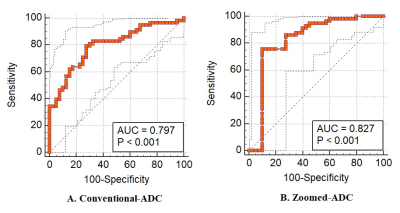
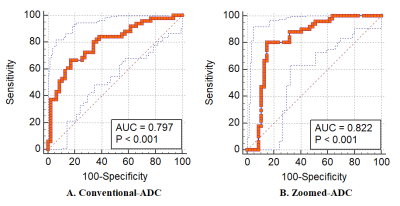
Ninety-eight patients (69.8 ± 7.5 years) were enrolled in this study. For patients with multifocal lesions, the lesions with the largest sizes according to DWI were included. Thus a total of 98 lesions were analyzed in this study, including 7 lesions in the G6 group (GS = 6), 31 lesions in the G7 group (GS = 7), 20 lesions in the G7+ group (GS > 7), and 40 lesions with benign lesions. Of all included lesions, 50% originated in the peripheral zone; the others originated in the transition zone. Zoomed DWI exhibited significantly reduced distortions of the prostate and reduced artifacts (P < 0.05 for both). The CNRs of the cancer lesions on the zoomed b1500 were not significantly different from those on the conventional DWI (conventional b1500) (96.5 ± 62.9 vs. 98.0 ± 68.7, P > 0.05). The CNRs of the cancer lesions on calculated zoomed b2000, however, increased significantly compared with the acquired zoomed b1500 (335.7 ± 199.6 vs. 96.5 ± 62.9, P < 0.05), but no significant differences were found among lesions in the G6, G7, or G7+ groups. Compared with the ADCs derived from conventional DWI, the ADCs of zoomed DWI were lower for all groups (P < 0.05 for all). Apart from the difference between the G6 and G7 subgroups, significant differences in ADCs were found among other subgroups by the conventional and zoomed techniques (P < 0.05, for all). With a threshold score of category 4 or greater on the prostate imaging reporting and data system (PI-RADS), the zoomed technique increased the sensitivity and negative predictive value for overall cancer as well as detection of clinically important cancer. Based on receiver operating characteristic curves, the AUC values for differentiating benign lesions from overall cancer were 0.827 (95% CI: 0.737-0.896) using ADCs derived from zoomed DWI, and 0.797 (95% CI: 0.704-0.872) using ADCs derived from conventional DWI (Figure 2). When differentiating benign lesions from clinically important cancer, the AUC values were 0.822 (95% CI: 0.732-0.892) for zoomed DWI, and 0.797(95% CI: 0.704-0.872) for conventional DWI (Figure 3).Conclusion
The results indicate that zoomed DWI can provide superior image quality in terms of reduced artifacts and higher CNR, as well as improved prostate cancer detection.Acknowledgements
No acknowledgement found.References
[1]. Brendle C, Martirosian P, Schwenzer NF, Kaufmann S, Kruck S, Kramer U, Notohamiprodjo M, Nikolaou K, Schraml C.Diffusion-weighted imaging in the assessment of prostate cancer: Comparison of zoomed imaging and conventional technique. Eur J Radiol. 2016 May;85(5):893-900
[2]. Tamada T1, Ream JM, Doshi AM, Taneja SS, Rosenkrantz AB.Reduced Field-of-View Diffusion-Weighted Magnetic Resonance Imaging of the Prostate at 3 Tesla: Comparison With Standard Echo-Planar Imaging Technique for Image Quality and Tumor Assessment. J Comput Assist Tomogr. 2017 Nov/Dec;41(6):949-956.
[3].Zhang Y, Holmes J, Rabanillo I, Guidon A, Wells S, Hernando D.Quantitative diffusion MRI using reduced field-of-view and multi-shot acquisition techniques: Validation in phantoms and prostate imaging. Magn Reson Imaging. 2018 Sep;51:173-181
Figures