4757
Radiopathological features of primary extragonadal endodermal sinus tumor1Henan Provincial People’s Hospital, People’s Hospital of Zhengzhou University, Zhengzhou, China, 2Department of MR Research China, GE Healthcare, Beijing 100000, China., Beijing, China
Synopsis
The extragonadal endodermal sac tumor (EEST) is an extremely rare malignant germ cell tumor and has a poor prognosis. Therefore, familiarity of the radiological characteristics of EESTs could help preoperative diagnosis and improve surgical management of patients. In this study, we investigate CT and MRI characteristics of 25 patients with EESTs correlated with pathological results, for better understanding and cognition in the diagnosis of EEST. Finally, we found that imaging features coupled with clinical data and the serum AFP check are helpful for the diagnosis of EEST and could improve the accuracy of the preoperative diagnosis.
Introduction
Endodermal sac tumor, also known as yolk sinus tumor, is a subtype of germ cell tumor which is rare and highly malignant. Most ESTs occur primarily in gonads such as ovaries and testes. The primary extragonadal endodermal sac tumors (EESTs) are extremely rare, which comprise about 10% to 20% of all ESTs (1,2). The most common extragonadal locations of EST are the mediastinum, sacrococcygeal region, retroperitoneum, cervix, head and neck, and stomach (1-4). Although EESTs have been reported, majority of prior studies regarding EESTs are case reports and do not supply the summary of their characteristic CT and MRI imaging features (2-7), which lead to difficulties in preoperative diagnosis. Therefore, we retrospectively analyzed the computed tomography (CT) and magnetic resonance imaging (MRI) features and clinical data of 25 patients with primary EESTs confirmed by pathology in the study and reviewed the related literature, so as to improve the diagnosis and differential diagnosis of EEST. To the best of our knowledge, this is the largest cohort of radiological reports of EESTs up to now.Methods
The clinical data, CT and MRI images of 25 patients with pathologically proved EESTs were retrospectively reviewed and summarized. Patient age, and the location, size, internal configuration, margin, density/signal, style of enhancement and surrounding infiltration of the lesions were evaluated.Results
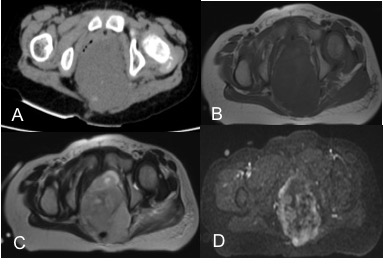
The locations of 25 EESTs were distributed in the mediastinum (n=12), sacrococcygeal region (n=9), sellar region (n=2), right frontal lobe (n=1), pineal region(n=1). 11 females and 14 males were included. The median age was 17.4 years (range, 1-41 years). All tumors were seen as oval or irregular masses with a mean size of 9.1 cm. 16 tumors revealed entirely solid masses and 9 tumors revealed cystic-solid masses. Intratumoral hemorrhage was seen in 6 tumors on CT images and 7 tumors on MRI images. Calcification was seen in 6 tumors. After contrast media administration, the solid part of the masses showed moderate to marked enhancement, while the cystic part of the masses showed no enhancement. Enlarged and distorted intratumoral vessels were seen in 17 tumors. The serum level of AFP of all the 25 cases were significantly higher than the normal level.Discussion
EEST is an extremely rare malignant tumor. Familiarity of its radiological characteristics may improve the accuracy of preoperative diagnosis. Nevertheless, a detailed report of the imaging descriptions of EEST with pathological correlation is very rare. In the study, we present the largest sample size of radiological studies of EESTs so far. EESTs are usually larger soft tissue masses and generally occur in central axis of the human body, such as mediastinum, sacrococcygeal region, pineal region et al. Mediastinal EESTs occurs mostly in young men; EESTs of sacrococcygeal region occurs mostly in young girls; Intracranial EESTs occurs mostly in children and adolescents. EESTs often accompanied by a clinically elevated serum AFP. On CT and MRI images, EESTs usually showed large, well-defined, uneven or solid-cystic masses with intratumoral hemorrhage, necrosis and cystic degeneration, significant heterogeneous enhancement, and enlarged intratumoral twisted vessels. However, the final confirm diagnosis still requires pathological examination.Conclusions
EEST has multiple characteristic imaging features. Imaging features coupled with clinical data and the serum AFP check may play an important role in the primary diagnosis of EEST and could improve the accuracy of the preoperative diagnosis.Acknowledgements
This research was supported by the NNSFC (81720108021, 81772009, 81601466, 81641168, 31470047), National Key R&D Program of China (YS2017YFGH000397), Scientific and Technological Research Project of Henan Province (182102310162) and the Key Project of Henan Medical Science and Technology Project (201501011).References
1. McKenney JK, Heerema-McKenney A, Rouse RV. Extragonadal germ cell tumors: a review with emphasis on pathologic features, clinical prognostic variables, and differential diagnostic considerations. Adv Anat Pathol 2007; 14:69–92
2. Haranoa K, Andoc M, Sasajimab Y, Yunokawaa M, Yonemoria K, Shimizua C, et al. Primary Yolk Sac Tumor of the Omentum: A Case Report and Literature Review. Case Rep Oncol 2012; 5(3):671–675
3. Filho BC, McHugh JB, Carrau RL, Kassam AB. Yolk sac tumor in the nasal cavity. Am J Otolaryngol 2008; 29:250–254
4. Nakhla SG, Sundararajan S. A rare case of primary anterior mediastinal yolk sac tumor in an elderly adult male. Case Rep Oncol Med. 2016; 2016:8961486
5. Lin SC, Li XH, Sun CH, Feng ST, Peng ZP, Huang SY, et al. CT Findings of Intrarenal Yolk Sac Tumor with Tumor Thrombus Extending into the Inferior Vena Cava: A Case Report. Korean J Radiol 2014;15(5):641-645
6.Papaioannou A, Porpodis K, Spyratos D, Zarogoulidis K. Yolk sac tumour in the anterior mediastinum. Pneumon 2013; 26 (4): 361–365
7. Li YK, Zheng Y, Lin JB, Xu GX, Cai AQ, Chen RW, et al. Radiological–pathological correlation of yolk sac tumor in 20 patients. Acta Radiol. 2016;57(1):98-106
Figures