4749
Prebiopsy mpMRI to Increase the Detection Rate and Reduce the Overdiagnosis of Prostate Cancer1Department of NMR, All India Institute of Medical Sciences, New Delhi, India, Ansari nagar, India, 2Department of Radio-diagnosis, RPC, All India Institute of Medical Sciences, New Delhi, India, Ansari nagar, India, 3Department of Radio-diagnosis, IRCH, All India Institute of Medical Sciences, New Delhi, India, Ansari nagar, India, 4Department of Urology, All India Institute of Medical Sciences, New Delhi, India, Ansari nagar, India, 5Department of Pathology, All India Institute of Medical Sciences, New Delhi, India, Ansari nagar, India, 6Present address.Department of Radiology, Chettinad Academy of Research and Education, Kelambakkam, Tamil Nadu, India
Synopsis
The results of the study showed that mpMRI guided in-bore biopsy has the potential to increase the detection rate of PCa. Prebiopsy mpMRI of prostate was used for identification of suspicious areas of malignancy which were targeted for PCa detection and reducing unnecessary biopsies. The detection rate was compared with TRUS guided 12 core biopsy. The data also indicated that using prebiopsy mpMRI may also help to reduce unnecessary biopsies. The PCa detection rate of in-bore mpMRI targeted biopsy was 53.84 % compared to 37.27% for TRUS guided biopsy.
Introduction
Prostate cancer (PCa) is most frequent malignancy in men over the age of 50 years worldwide1. Many clinically insignificant PCa screened by PSA and DRE, may result on to overdiagnosis and overtreatment. The aim of this study was to evaluate role of prebiopsy mpMRI of prostate for finding suspicious areas for detection of PCa and reducing unnecessary biopsies using PIRADS scores ≤ 3.Method
Patients were recruited based on PSA >4 ng/ml and abnormal DRE. MR investigations were carried out at 3.0 T MRI system, using mp-MRI (T1-WI, T2-WI, DWI and DCE-MRI). Group I consist of 52 patients, (mean age: 66.2 ±7.6 years, mean PSA: 20.1 ±19.8ng/ml) who underwent mpMRI guided targeted in-bore biopsy while Group II had 110 patients who underwent only TRUS guided 12 core systematic biopsy procedure. All Group I patients had mpMRI and reporting according to the PIRADS version 2. T2W images were acquired with the following parameters: TRof 6100 ms,TE of 100 ms, FOV = 240 x 240 mm, and slice thickness 3 mm, DWI was carried out using seven b-values 0- 200, 400,800,1000,1500, 2000 s/mm2. ADC values of hypointense area which is suspicious of malignancy were calculated from ADC map. For DCE-MRI, 20 ml Gadolinium was injected at a rate of 3ml/s. Patients having PIRADS ≥ 3 scores underwent in-bore biopsy, using a DynaTrim ( Invivo, USA) biopsy device with needle guide and DynaCad software. Biopsy was carried out by transrectal approach.Results
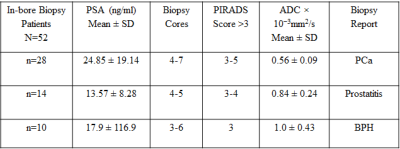
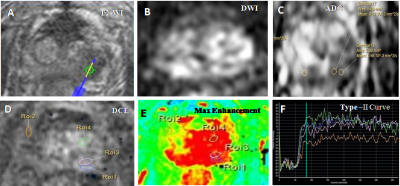
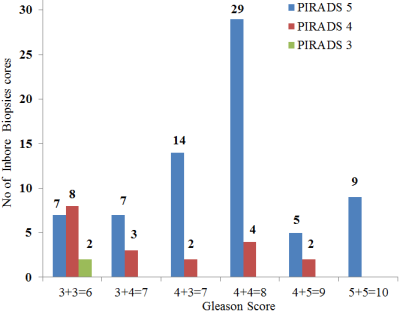
Our study demonstrated that mpMRI accurately identified suspicious areas of lesion and MR guided inbore biopsy helped to target these areas with accuracy (Figure 1). These targeted lesions with PIRADS scores ≥ 3 were correlated with the histopathological findings (Figure 2). The mean ADC for malignant lesions (0.56±0.09x10-3 mm2/s) lower compared to prostatitis (0.84±0.24x10-3 mm2/s,) and BPH (1.0±0.43x10-3 mm2/s). The use of ADC may reduce the number of unnecessary biopsies cores. The PCa detection rate of in-bore targeted biopsy was 53.84 % compared to 37.27% for TRUS biopsy. Using the in-bore biopsy method, 270 core biopsies were collected from 52 patients (~5 cores per patient). 140 core biopsies were from prostate cancer patients and out of these, 92 (65 %) were positive for malignancy on histopathology (Figure 1). Out of all 52 patients who underwent mpMRI guided biopsy, 28 were positive for cancer with Gleason scores: 6(3+3), 7(3+4), 7(4+3), 8(4+4) and 9(4+5),10 (5+5) while 14 patients had prostatitis and 10 patients had BPH (Table 1). 110 patients who underwent TRUS guided 12 core biopsies revealed that 41 were positive for PCa.Discussion
In this study we demonstrated that the use of mpMRI guided in-bore biopsy for increased detection rate of PCa which reduces the limitation associated with TRUS-guided biopsy especially for lesions located in the central and anterior regions of the prostate. Our finding suggests that using ADC values of suspicious area before the biopsy may help to accurately target the ROI for biopsy and also to reduce unnecessary biopsies. In addition mpMRI reporting PIRADS-v2 score correlated strongly with high-grade PCa.Conclusion
mpMRI guided targeted in-bore biopsy has the potential to significantly increased the detection rate of prostate cancer. In addition, the targeted biopsy approach may also result in reducing unnecessary biopsies, thereby improving the patient experience and comfort level associated with biopsy procedureAcknowledgements
NRJ thanks SERB, Government of India funding under FIST program (SR/FST/LSI-569/2013) and J.C. Bose Fellowship.References
1. Ferlay J, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015 Mar 1; 1;136(5) E359-86.
2. V. Kasivisvanathan, et al. MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis: N Engl J Med. 2018 May 10; 378:1767-77.