4748
Baseline MRI detected lateral lymph node as a prognostic factor: a cohort study in pN0 low risk rectal cancer
Rui-Jia Sun1, Lin Wang1, Xiao-Ting Li1, Qiao-Yuan Lu1, Xiao-Yan Zhang1, and Ying-Shi Sun1
1Beijing Cancer Hospital, Beijing, China
1Beijing Cancer Hospital, Beijing, China
Synopsis
Baseline MRI detected lateral lymph node was associated with poor prognosis in patients with pN0 low risk rectal cancer. For patients with MR detected lateral lymph node of a short axis at least 8mm, the present clinical strategies may be unlikely sufficient.
Background:
It is highly controversial that how to deal with the lateral lymph node metastasis in patients with rectal cancer. Although lateral lymph node can be detected by preoperative MRI, the metastasis status cannot be accurately determined following standard total mesorectal excision (TME) in low risk patients. This study was to assess the correlation between preoperative MRI detected lateral lymph node (LLN) features and prognosis in patients with non-preradiated low recurrence risk rectal cancers.
Materials and Methods:
This retrospective study included 593 low risk rectal cancers underwent TME without neoadjuvant chemo-radiatherapy from January 2013 to December 2015. The features of the largest LLN were retrospectively reviewed on preoperative MRI. The relationship of MR-LLN features with overall survival, metastasis-free survival, and local relapse-free survival was analyzed.
Results:
A total of 593 patients including 415 cases of pN0, 86 cases of pN1 and 92 cases of pN2 were enrolled in this study. In pN0 patients, at least one visible LLN was detected in 104 patients on primary MRI. The MR-T staging, postoperative therapy status, the presence of MR-LLN, and short axis (SA) of MR-LLN were significantly correlated with the recurrence in pN0 patients (all p<0.05). The OS and MFS were significantly lower in patients with MR-LLN SA≥8mm than SA<8mm (p<0.01, HR=4.35, 95%CI=1.48-12.77). The OS and MFS of patients with pN0-LLN(+) and SA≥8mm were similar to pN2-LLN(-) patients. The location of MR-LLN showed no significant impact on prognosis.
Conclusion:
For low-risk rectal cancers without neoadjuvant chemoradiatherapy, the presence of MR-LLN is associated with poor prognosis. The pN0-LLN(+) SA≥8 mm patients might be concerned as pN2 patients and receive more intensive neoadjuvant or adjuvant treatment.
It is highly controversial that how to deal with the lateral lymph node metastasis in patients with rectal cancer. Although lateral lymph node can be detected by preoperative MRI, the metastasis status cannot be accurately determined following standard total mesorectal excision (TME) in low risk patients. This study was to assess the correlation between preoperative MRI detected lateral lymph node (LLN) features and prognosis in patients with non-preradiated low recurrence risk rectal cancers.
Materials and Methods:
This retrospective study included 593 low risk rectal cancers underwent TME without neoadjuvant chemo-radiatherapy from January 2013 to December 2015. The features of the largest LLN were retrospectively reviewed on preoperative MRI. The relationship of MR-LLN features with overall survival, metastasis-free survival, and local relapse-free survival was analyzed.
Results:
A total of 593 patients including 415 cases of pN0, 86 cases of pN1 and 92 cases of pN2 were enrolled in this study. In pN0 patients, at least one visible LLN was detected in 104 patients on primary MRI. The MR-T staging, postoperative therapy status, the presence of MR-LLN, and short axis (SA) of MR-LLN were significantly correlated with the recurrence in pN0 patients (all p<0.05). The OS and MFS were significantly lower in patients with MR-LLN SA≥8mm than SA<8mm (p<0.01, HR=4.35, 95%CI=1.48-12.77). The OS and MFS of patients with pN0-LLN(+) and SA≥8mm were similar to pN2-LLN(-) patients. The location of MR-LLN showed no significant impact on prognosis.
Conclusion:
For low-risk rectal cancers without neoadjuvant chemoradiatherapy, the presence of MR-LLN is associated with poor prognosis. The pN0-LLN(+) SA≥8 mm patients might be concerned as pN2 patients and receive more intensive neoadjuvant or adjuvant treatment.
Acknowledgements
This work was supported by Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (No.ZYLX201803),Beijing Municipal Administration of Hospitals’ Youth Program (Code: QML20181103) and This study was supported by Beijing Municipal Science & Technology Commission (Z171100001017102).References
No reference found.Figures
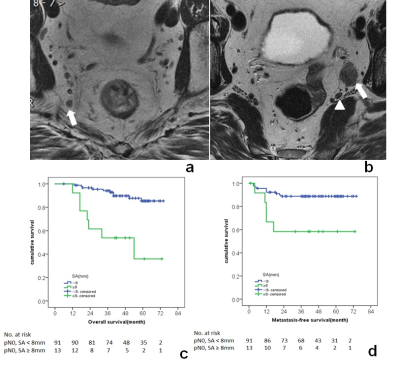
(a)(b)Examples of MR-detected lateral lymph nodes in different regions. (a) In a pT2N0 male patient, MR-detected a 5x6mm lymph node (arrow) located in the internal iliac region. (b) In a pT2N0 female patient, MR-detected a 12x15mm lymph node (arrow) located in the obturator region. The internal iliac artery (arrow head) was identified behind the enlarged lymph node. (c)(d)Kaplan-Meier curves for the association between short axis of the largest MR-LLN and the (c) OS and (d) MFS in pN0 patients.