4704
An In-vivo Assessment of Regional Brain Temperature during Whole-body Cooling for Neonatal Encephalopathy
Tai-Wei Wu1, Jessica Lee Wisnowski1, Rachel Chapman1, Marvin D Nelson2, Benita Tamrazi2, and Stefan Bluml2,3
1Neonatology, Children's Hospital Los Angeles/USC, Los Angeles, CA, United States, 2Radiology, Children's Hospital Los Angeles/USC, Los Angeles, CA, United States, 3Rudi Schulte Research Institute, Santa Barbara, CA, United States
1Neonatology, Children's Hospital Los Angeles/USC, Los Angeles, CA, United States, 2Radiology, Children's Hospital Los Angeles/USC, Los Angeles, CA, United States, 3Rudi Schulte Research Institute, Santa Barbara, CA, United States
Synopsis
Regional brain temperatures in newborns hypoxic-ischemic encephalopathy (HIE) were measured during whole-body hypothermia (TH) to test the hypothesis that brain temperature profile is non-homogenous and is related to pattern or severity of brain injury. We found that whole body hypothermia was effective in cooling deep brain structures, while superficial structures were warmer and significantly higher than rectal temperature. It was also observed that infants with more severe brain injury exhibited higher brain temperatures without regional temperature differences.
Introduction
Therapeutic hypothermia (TH) is modestly effective in reducing death and severe disability for neonatal HIE [1], but its neuroprotective properties rely on timely lowering of brain temperature [2,3]. Depending on the method of cooling and presence/absence of brain injury, a temperature gradient can form between deep and peripheral brain, with deep structures being warmer [4,5]. The resistance of local brain structures to TH may not be clinically obvious, because of the lack of clinically feasible brain temperature monitoring and the reliance of core body temperature as a surrogate measure of brain temperature. Advances in MR science allows for non-invasive measurement of regional brain temperature to an accuracy of approximately 0.2°C [6,7] (Fig. 1).Methods
Fifty-three newborns with birth complications and HIE (22 males and 31 females, mean gestational age 38.3±2 weeks, birthweight 3247±630g) were enrolled prospectively. MR spectra of basal ganglia (BG), thalamus (Thal), cortical gray matter (GM), and white matter (WM) were acquired during TH. Depth of regions of interest was measured as the shortest distance from the center of the voxel to the outer edge of the cranium. The targeted rectal temperature (33.5±0.5°C) was monitored and maintained during the MR examination. All MR measurements were performed on a 3T clinical scanner using single voxel PRESS (TE=35ms, TR=2s, 128 averages). Regional brain tissue temperatures were calculated from the chemical shift difference between water signal and metabolites in the MR spectra after performing calibration measurements. Overall difference in regional temperature was analyzed by mixed effects model and temperature among different patterns and severity of injury on MRI were also analyzed. Correlation between temperature and depth of brain structure was analyzed using repeated measures correlation. MR spectra were acquired at mean age of 2.2±0.6 days. A total of 201 MR spectra were included in the analysis.Results
Overall, Thal, the deepest structure (36.4±2.3 mm from skull surface), was lowest in temperature (33.2±0.8°C, compared to BG: 33.5±0.9°C; GM: 33.6±0.7°C; WM: 33.8±0.9°C, all p<0.001, Fig. 2). Temperatures in more superficial GM and WM regions (21.9±2.4 and 21.5±2.2mm) were significantly higher than the rectal temperatures (33.4±0.4°C, p<0.03). There was a significant negative correlation between temperature and depth of brain structure (rrm=0.36, p<0.001).When severity of injury was included in the analysis, infants with more severe brain injury on MRI had a significantly higher brain temperature than those without evidence of brain injury (Mann Whitney test: mean rank 82.5 vs. 65.8, p =0.02, Fig. 3). In those with “normal” pattern of injury (n=30), there was a significant difference in regional brain temperature, [F(3.01, 77.46)=3.99, fixed effect p=0.01] with post-hoc multiple comparisons revealing significant temperature difference between Thal and GM (33.05 ± 0.89°C vs. 33.58 ± 0.70°C, p<0.01) and Thal and WM (33.05 ± 0.89°C vs. 33.78 ± 0.98°C, p<0.01). However, there was no significant regional temperature difference among those with central BG-T injury [F(1.82, 14.10), p=0.10] or WS pattern of brain injury [F(2.60, 28.60)=3.03, p=0.05]. There was also no significant difference in regional temperature among those with severe injury on MRI [F(2.16,23.75, p=0.11)].Discussion
Using MR thermometry, we measured temperatures of various brain structures that were at risk of hypoxic-ischemic injury and correlated the measurements to physical depth of tissue, and characteristic of brain injury. The results of this investigation revealed that whole-body TH effectively lowered deep grey matter structures, while temperatures of more superficial structures such as GM and WM were slightly, but significantly higher than rectal temperatures. Effective cooling of deep structures by whole body TH may be related to the distribution of blood supply in the core grey matter. The dissipation of heat in deep cerebral tissues is largely dependent on the thermal gradient between brain tissue and surrounding arterial blood temperature. In normal physiological conditions, cerebral arterial blood flow acts as the heat sink absorbing heat from surrounding tissue. During whole body TH, cooled systemic arterial blood circulates through the circle of Willis before reaching watershed regions that are more peripheral in location.Conclusions
Deep brain structures were effectively cooled by whole body hypothermia. Infants with more severe brain injury exhibited higher brain temperatures without regional temperature differencesAcknowledgements
Rudi Schulte Research InstituteReferences
1. Douglas-Escobar M, Weiss MD. JAMA Pediatr. 2015;169:397-403. 2. Gunn AJ et al. J Clin Invest. 1997;99:248-56. 3. Laptook AR et al. JAMA. 2017;318:1550-60. 4. Laptook AR et al. Pediatrics. 2001;108:1103-10. 5. Iwata O et al. Pediatr Int. 2003;45:163-8. 6. Childs C et al. Magn Reson Med. 2007;57:59-66. 7. Cady EB et al. NMR Biomed. 2011;24:865-72.Figures
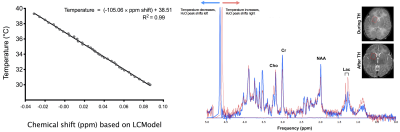
Fig. 1, Left: For calibration, MR spectra from GE BRAINO phantom were acquired at different temperatures and processed with fully automated LCmodel software (Provencher Inc, Ontario, CA). Right: In vivo example generated from spectra acquired during TH (blue) and after TH (red) in the same patient. There is a larger frequency difference between the water peak and the metabolite spectrum during cooling which indicates lower tissue temperature.
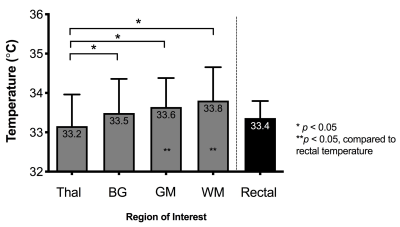
Fig. 2: Regional brain temperature was assessed during therapeutic hypothermia. There was a significant difference in temperature among Thal, BG, and GM, denoted by *. There was also a significant difference between temperature of peripheral brain regions (GM and WM) and the rectum, denoted by **. Numbers within bars represent mean and error bars are standard deviation. Thal=thalamus; BG=basal ganglia; GM=occipital parietal gray matter; WM=white matter.
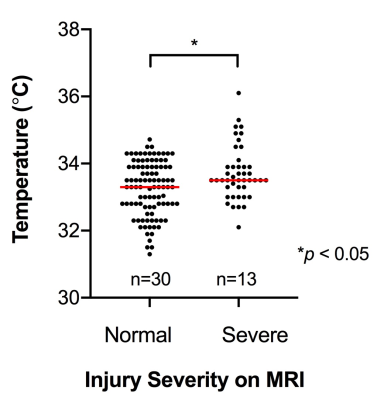
Fig. 3: There was a significant difference in brain temperature between infants without injury and with severe injury on MRI based on Mann-Whitney U test. Both cohorts were non-normal in distribution. Dark horizontal bar represents the median brain temperature. Of note, there was not significant difference between rectal temperatures between the two groups, p=0.64.