4691
Combining different high resolution MR vessel imaging sequences in pediatric medulloblastoma survivors: Be faster than the stroke event1Neuroradiology, University Medical Center Mainz, Mainz, Germany, 2Pediatric Hematology/ Oncology/ Hemostaseology, University Medical Center Mainz, Mainz, Germany
Synopsis
Imaging cerebro- vasculopathy after radio-chemotherapy in pediatric Medulloblastoma survivors, by assessing internal media thickening of the external carotid artery through ultrasound and comparing black blood high resolution vessel wall imaging sequences with TOF-MR-Angiography, Volume Interpolated GRE/±CE and T2 tse fat saturated sequences. The underlying study indicates a superiority of black blood sequences in early detection of vascular changes, which might lead to vasculopathy, in comparison to the commonly used sequences. Thus follow-up MRI protocols might include black blood vessel wall images.
Background
Over the last 20 years therapy regimes for pediatric medulloblastoma (MB) have improved, with this former pediatric medulloblastoma survivors are increasing1. Life limiting factor for these population are now late sequelae, including cerebrovasculopathies, after radio-chemotherapy (RCT)2. Therfore early dection and monitoring of cerebrovasculopathies before clinical onset is of interest and importance. This study is assessing cerebrovascular changes for the ICA, ACA, MCA, PA, VA and BA separately, by using high resolution MR vessel wall imaging. Hereby comparing commonly used vessel imaging sequences, like time of flight (TOF)-MR Angiography (MRA), Volume Interpolated GRE/±CE and T2 tse fat saturated sequences with high resolution vessel wall sequences (2D T2 and 2D black blood T1±CE). The future objective is to implement standardized follow-up imaging protocols for pediatric MB survivors. Thus the aim of this study was i) to assess the benefit of including vessel wall imaging sequences in follow-up protocols, herby assessing the feasibility for different intracranial vessels, ii) to compare the findings imaged by vessel wll sequences with findings imaged by standard vessel sequences.Methods
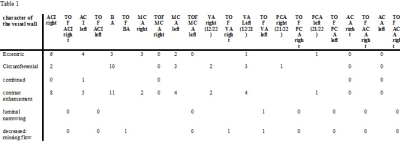
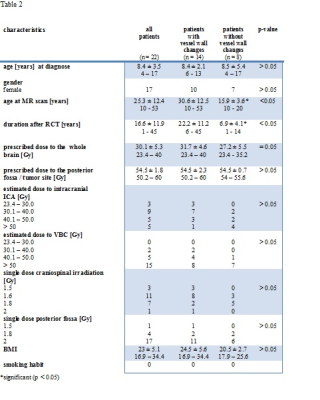
Twenty two former pediatric MB survivors (mean age [years]: 25.8, mean age: at first time RCT: 8.4) underwent MRI examination at 3 Tesla MR scanner. MRI protocol included following vascular sequences: TOF-MRA (3D), Volume Interpolated GRE/±CE (3D, SD 1mm), T2 tse fat saturated (2D, SD 3 mm), high resolution vessel wall sequences: (T2 tse (2 D, SD 2 mm), T1±CE (2 D, SD 2mm)). Diffusion-weighted (DWI) MR images have included, ruling out silent stroke. Vessel wall thickening, CE of the vessel wall and luminal narrowing, alterations of vessel flow and missing vessel flow (for TOF-MRA and Volume Interpolated GRE sequences) were assessed by two experienced neuroradiologists’. The internal media thickening (IMT) of the external carotid artery was examined, through ultrasound. Radiation whole head dose and boost, dose to the ACI, MCA and to the vertebro-basilar system (VBS), was extracted separately. Clinical data and disability was evaluated. Multivariate regression analysis has been performed, assessing age at first time RCT and radiation dose as independent predictors for developing vessel wall changes within the MCA, ACI and VBS. Results: In 14/22 patients’ vessel wall changes were observed, while the VBS was most affected (13/22). Images of the VA, ACA and PCA wall, was not assessable for all 22 patients, due to too small imaging size or artifacts. Decreased or missing vessel flow signal in TOF-MRA and T1 Volume Interpolated GRE was observed for one patient. Detailed results, capturing vessel wall thickening, wall CE, luminal narrowing, decreased and/or missing vessel flow, captured for every vessel separately is shown in table 1. IMT of the external ACI was examined for 19 out of 22 patients, with a mean IMT for the right (left) side of 0.46 mm, 0.45 mm, respectively. Radiation dose and fractionation was available for 21/22 patients. Grade of disability did not correlate with vascular changes. Further clinical data, including radiation dose is shown in table 2. Although neither dose nor age at first time RCT showed a significant correlation with developing vessel wall changes, a tendancy for dose related vessel wall changes was observed for the vertebrobasilar system and the internal carotid artery (p = 0.1).Discussion
Vascular disease is frequently observed in former pediatric tumor patients3. Aim of this study was to compare high resolution vessel wall MR imaging sequences and routinely used vessel sequences, for imaging vascular changes at an early stage before clinical onset. Black blood T1±CE sequences show vascular changes with in the ICA, BA and MCA wall, whereas these changes are not seen in the well-established vessel sequences. Only for one patient vessel changes could be observed with TOF-MRA, T2 tse fat sat and Volume Interpolated GRE/±CE sequences, but this patient had already a major stroke event in the PA territory. Many studies suggest a relationship between radiation dose and the risk of stroke in pediatric patients treated by cranial radiotherapy 4, 5 . This is emphazied by our results, as the majority of vasculopathy was found for the VBS and with this in the field of additional radiation boost. The results of this study, indicate that well established vessel imaging sequences do not show vascular changes at an early stage in comparison to T1 black blood sequences6. However, vessel wall sequences do not sufficiently capture vessel wall changes within in the ACA and PA. Further improvement of vessel imaging sequences are needed.Conclusion
While cerebrovascular changes after RCT are imaged at an early stage through T1 black blood sequences, routinely used vessel sequences show vascular changes only at a later stage, when stroke events have already happened. Furthermore an increased extracranial carotid IMT is showing prevalence for carotid artery disease. Given, late sequelae after RCT has become life limiting factor for former pediatric medulloblastoma survivors, it is of interest to detect vasculopathies at an early stage. Black blood sequences are superior in detecting those, giving best monitoring opportunities and the possibility for early intervention. Further studies are needed to gain more insight.Acknowledgements
No acknowledgement found.References
1. Gesellschaft für Pädiatrische Onkologie und Hämatologie. S1 Leitlinie der Gesellschaft für Pädiatrische Onkologie und Hämatologie: Medulloblastom im Kindes- und Jugendalter. 2012. Available at: http://www.awmf.org/uploads/tx_szleitlinien/025-009l_S1_Medulloblastom_2012-11.pdf. Accessed October 9, 2016.
2. Meeske KA, Siegel SE, Gilsanz V, et al. Premature carotid artery disease in pediatric cancer survivors treated with neck irradiation. Pediatric blood & cancer. 2009;53:615-621.
3 . Bowers DC, Liu Y, Leisenring W, et al. Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2006;24:5277.
4. Bowers DC, Liu Y, Leisenring W, et al. Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2006;24:5277.
5. Mueller S, Fullerton HJ, Stratton K, et al. Radiation, atherosclerotic risk factors, and stroke risk in survivors of pediatric cancer: a report from the Childhood Cancer Survivor Study. Int. J. Radiat. Oncol. Biol. Phys. 2013;86:649-655.
6. Mossa-Basha M, Hwang WD, Havenon A de, et al. Multicontrast High-Resolution Vessel Wall Magnetic Resonance Imaging and Its Value in Differentiating Intracranial Vasculopathic Processes. Stroke. 2015;46:1567-1573.
Figures
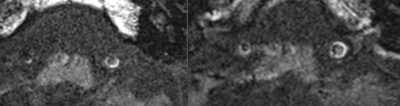
Left: Black blood T1 vessel wall sequence: showing vessel wall thickening of the verterbal artery
Right: Black blood T1 CE vessel wall sequence: showing a contrast enhancement of the VA vessel wall (both sides)
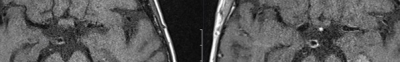
Left: Black
blood T1 vessel wall sequence: showing vessel wall thickening of the basilar artery
Right: Black
blood T1 CE vessel wall sequence: showing a contrast enhancement of the basilar artery wall and the medial cerebral artery wall (both sides)