4689
Investigation of cerebral small vessel disease and impacting clinical factors in young patients with symptomatic cerebral infarction1the First Affiliated Hospital of Dalian Medical University, Dalian, China, Dalian, China, 2GE Healthcare, MR Research China, Beijing, Beijing, China, Beijing, China
Synopsis
In this study, we selected the first infarction of young patients as a study object, retrospective analysis of young cerebral infarction, senile cerebral infarction and healthy young people's brain cerebral small vessel diseases (CSVD) imaging findings, and further analysis of its clinical influencing factors to further explore the etiology of infarction in young patients. We found that CSVD often occurs in young and elderly patients of cerebral infarction, while it is more frequent and serious in elderly patients. Hypertension, smoking, and age may be factors influencing cerebral small vessel disease in young patients with cerebral infarction.
Introduction
Cerebral infarction in young patients refers to cerebral infarction with an onset age of 18 to 45 years old, which accounts for about 5% of the overall population. However, an increasing trend of the occurrence has recently been observed[1]. Cerebral small vessel disease (CSVD) refers to a series of pathological processes affecting the structure or function of small blood vessels in the brain, including arteries, arterioles, venules and capillaries. It is mainly characterized by enlarged perivascular space (EPVS), lacunar infarction (LI), white matter hyperintense (WMH), cerebral microbleeds (CMBs) and brain atrophy. CSVD is considered to be a common manifestation of senile cerebrovascular disease, and has a clear correlation with clinical symptoms and characteristics[2]. At the present, limited studies are available for investigating the CSVD in young patients with cerebral infarction have CSVD and the impacting clinical factor, which is the aim of this explorative study.Materials and Methods
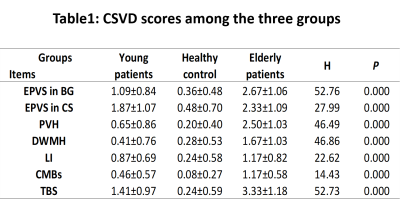
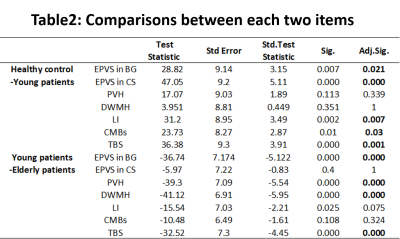
A total of 111 cases of primary acute cerebral infarction were enrolled in this study, including 54 cases of young cerebral infarction (43 men and 11 women; mean age, 38.41±4.66 yrs) with the age less than 45 years old and 57 cases of senile cerebral infarction (37 men and 20 women; mean age, 68.96±10.28 yrs). Ethical approval was obtained in the local institute and consent forms were obtained. Clinical data of all patients at admission were collected, including blood pressure, fasting blood glucose, total cholesterol, triglyceride, high density lipoprotein, low density lipoprotein, homocysteine, and smoking and drinking. All subjects underwent routine MR sequences (including T1WI, T2WI and T2 FLAIR) and DWI on 1.5T MRI scanner. Two experienced radiologists evaluated the CSVD independently as the following : enlarged perivascular spaces (EPVS) were counted and scored in basal ganglia (BG) and centrum semiovale (CS);, lacunar infarction (LI) were counted, white matter hyperintensity lesions (WMH) were graded and recorded. To reduce the bias in assessment of the severity of the patient's CSVD, the patient's EPVS, WMH, LI, and CMBs scores were collectively accounted to derive the total burden scores of CSVD (TBS) (0-4 scores). The interclass correlation coefficient (ICC) was used to evaluate consistency between the two observers. The Kruskal-Wallis H test were used to compare the ranked data between groups. Correlation between CSVD and clinical factors were assessed by Spearman correlation analysis.Results
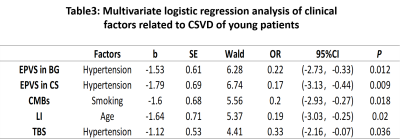
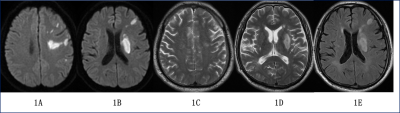
Images of a patient with acute cerebral infarction in the left frontal lobule and basal ganglia are shown in Figure 1. The data of CSVD evaluated by the two observers were in good agreement (all ICC > 0.75). Difference among the scores of the three groups was observed (P < 0.001) Based on a pair-to-pair comparison, there was significant difference in TBS among the three groups (P < 0.001 after adjustment). The score of the infarction group was significantly higher than that of the control group, but significantly lower than the aged group. (Table1-2) Hypertension was observed as the influencing factor of EPVS and the influencing factors of TBS (P<0.05). Smoking was the influencing factor of CMBs (P<0.05). LI was closely related to age (P < 0.05) (Table 3).Discussion and conclusions
In this study, it was found that TBS in the young patients group was significantly higher than that of healthy control, but lower than the aged group, indicating that cerebral small vessel disease may be common in young patients with acute cerebral infarction. TBS was used in this study to for overall assessment of the CSVD, which may fully reflect the overall impact on the brain compared to the characteristics of single cerebral small vessel disease[3]. In addition, this study showed hypertension might be the strongest vascular risk factor for CSVD. Thus cautions shall be paid for hypertension in young group for prevention of CSVD at older age.Acknowledgements
References
[1] Huang Y, Yang S, Jia J. Factors Related to Long-Term Post-Stroke Cognitive Impairment in Young Adult Ischemic Stroke[J]. Medical Science Monitor International Medical Journal of Experimental & Clinical Research,2015,21:654-660.
[2] Pinter D, Enzinger C, Fazekas F. Cerebral small vessel disease, cognitive reserve and cognitive dysfunction[J]. Journal of Neurology,2015,262(11):2411-9.
[3] Staals J , Makin S D J , Doubal F N , et al. Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden[J]. Neurology, 2014, 83(14):1228-1234.