4665
Early developmental differences of white matter tracts in preterm infants with brain injury1Department of Radiology and Biomedical Imaging, University of California, San Francisco, CA, United States, 2Department of Neurology and Pediatrics, University of California, San Francisco, CA, United States
Synopsis
We detected early developmental differences of white matter tracts in preterm infants with brain injury (BI). Nineteen preterm infants underwent two MRI scans. Microstructural development was analyzed combining conventional diffusion parameters and advanced NODDI parameters . We found BI preterm infants showed higher ODI in internal capsule, which was positively correlated with brain injuries severity; during the longitudinal period, most of the tracts in non-injured preterm infants had increased FA and Vic, decreased MD and ODI, while in BI preterm infants, only a few tracts developed. This study indicated white matter development was different in preterm infants with and without BI.
Introduction
Infants who born prematurely are often particular susceptible to brain injuries (BI), such as intraventricular hemorrhage (IVH) and periventricular leukomalacia (PVL). These brain injuries may disrupt the normal progression of brain development, especially for the white matter1. Altered microstructural organization has been demonstrated in many fiber tracts in preterm infants2, however, we still know little about the white matter maturation pattern in preterm infants with BI. Diffusion magnetic resonance imaging (dMRI) can be used to measure the microstructural organization of white matter non-invasively. Conventional diffusion tensor parameters including fractional anisotropy (FA) and mean diffusivity (MD), reflect the directional restriction of diffusion and degree of overall diffusion. Recently developed model such as Neurite Orientation Dispersion and Density Imaging (NODDI) allows a more direct examination of underlying cellular microstructural properties of the diffusion signal compared with traditional diffusion parameters3. In the current study, we aimed to investigate microstructural development in preterm infants with BI combining conventional diffusion parameters (FA and MD) and advanced NODDI parameters (neurite density index, Vic and orientation dispersion index, ODI).Methods
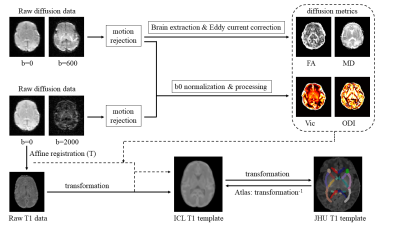
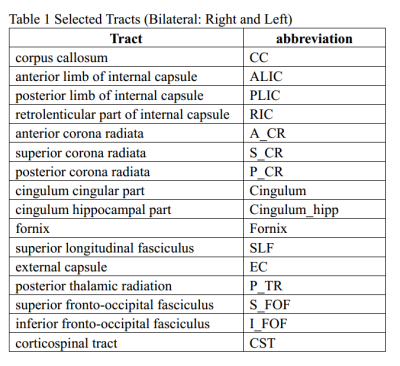
Nineteen preterm infants, born prematurely between 24 and 32 gestational weeks (mean, 28.9 ± 2.3 weeks) underwent two MRI scans at gestational age (GA) in 29~34 weeks (mean, 32.1±1.4 weeks, MRI-1) and 34~42 weeks (mean, 36.2±2.0 weeks, MRI-2) respectively. Radiologic assessments were completed by board certified neuroradiologists, using previously published IVH and PVL scoring systems. The infants were divided into 2 groups: 9 infants with BI and 10 infants with normal-appearing brains. MRI scanning includes: (1) structural 3D sagittal T1 weighted imaging; (2) whole-brain diffusion tensor imaging (one b=0 and 30 noncollinear directions with b=600s/mm2); (3) whole-brain high angular high angular resolution diffusion imaging (one b=0 and 55 noncollinear directions with b=2000s/mm2).Images were processed using pipeline detailed in Figure 1. We fitted four diffusion metrics (FA, MD, Vic, ODI), all these metrics were normalized to the Imperial College London (ICL) T1 template. Atlas derived from the Johns Hopkins University (JHU) neonatal template was warped onto ICL T1 template. Sixteen white matter tracts were selected as region of interesting (ROI) (Table1).
Two sample t-test was used to compare the difference between BI and non-injured preterm infants. Paired t-test was used to compare the WM diffusion parameter changes between MRI-1 and MRI-2. Correlation analysis was used to explore the relationships between diffusion metrics and BI severity.
Results
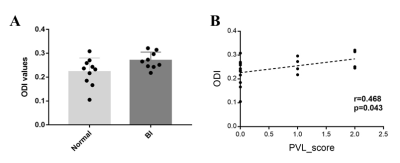
There was no difference between groups in birth GA (p=0.696), GA at MRI-1 (p=0.137) and GA at MRI-2 (p=0.077).Comparisons of four diffusion metrics in white mater tracts showed that BI preterm infants had higher ODI in right posterior limb of internal capsule (PLIC_R) than non-injured preterm infants (p < 0.05, Figure 2A). ODI in PLIC_R was positively correlated with brain injury severity (r=0.468, p=0.043, Figure 2B).
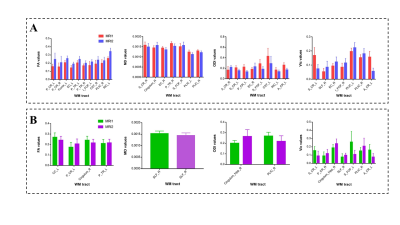
In the group of non-injured preterm infants, most of the fibers showed increased FA and Vic, decreased MD and ODI (Figure 3A). Selected results shown in Figure 3 reached statistical significance of p < 0.05. The group of BI preterm infants showed differences in diffusion patterns, in comparison with non-injured preterm infants (Figure 3B). For example in the PLIC_R, BI preterm infants only showed decreased ODI, and non-injured preterm infants showed increased FA, Vic and decreased MD.
Discussion
In the present study, we combined traditional diffusion parameters and advanced diffusion metrics to investigate the microstructural organization in preterm infants with and without BI, and also explored the white matter developmental patterns. We found that: (1) in BI preterm infants, higher ODI was observed in PLIC, which was positively correlated with brain injuries severity; (2) during the longitudinal period, most of the tracts in non-injured preterm infants had increased FA and Vic, decreased MD and ODI, which indicated a well development situation, while in BI preterm infants, only a few tracts developed, and the developmental mode was different from the non-injured preterm.Increased FA and decreased MD are reflective of mature microstructural organization of white matter fiber tracts4. However, DTI parameters cannot sensitively distinguish between different cellular properties including myelination, axon density, and axon coherence or geometry5. NODDI has the potential to provide a more specific axon density and dispersion of axon orientation, which can be related to the typical children development and better motor performance6, 7. In line with these previous studies, we found higher FA and Vic, lower MD and ODI during early brain development for non-injured preterm infants, which may indicate normal development. This will have to be followed up by neurobehavioral exams at a later time point.
We also observed higher ODI in PLIC in BI preterm infants. Internal capsule often characterized by the lower dispersion, the higher ODI may reflect the delayed maturation. Additionally, ODI in internal capsule was positively correlated with brain injuries severity, which further indicate increased injury is associated with increased developmental delays. In non-injured preterm infants’ internal capsule, increased FA, Vic, and decreased MD suggested the normal myelination and neurite formation. While in BI infants, development of internal capsule only correlated with decreased ODI, reflected the remodeling of axon geometry. These results suggest that the developmental trajectory in BI infants is different from those preterm infants without injury.
Acknowledgements
References
1. Miller SP, Cozzio CC, Goldstein RB, et al. Comparing the diagnosis of white matter injury in premature newborns with serial MR imaging and transfontanel ultrasonography findings. AJNR Am J Neuroradiol. Sep 2003;24(8):1661-1669.
2. Pandit AS, Ball G, Edwards AD, Counsell SJ. Diffusion magnetic resonance imaging in preterm brain injury. Neuroradiology. Sep 2013;55 Suppl 2:65-95.
3. Zhang H, Schneider T, Wheeler-Kingshott CA, Alexander DC. NODDI: practical in vivo neurite orientation dispersion and density imaging of the human brain. Neuroimage. Jul 16 2012;61(4):1000-1016.
4. Murner-Lavanchy IM, Kelly CE, Reidy N, et al. White matter microstructure is associated with language in children born very preterm. Neuroimage Clin. 2018;20:808-822.
5. Jones DK, Knosche TR, Turner R. White matter integrity, fiber count, and other fallacies: the do's and don'ts of diffusion MRI. Neuroimage. Jun 2013;73:239-254.
6. Kelly CE, Thompson DK, Chen J, et al. Axon density and axon orientation dispersion in children born preterm. Hum Brain Mapp. Sep 2016;37(9):3080-3102.
7. Lebel C, Deoni S. The development of brain white matter microstructure. Neuroimage. Nov 15 2018;182:207-218.
Figures