4662
Left inferior fronto-occipital fasciculus is key anatomical location of cognitive delay in preterm infants with mild white matter injury1Department of Diagnostic Radiology, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China, 2MR Research China, GE Healthcare, Beijing, China, 3Department of Diagnostic Radiology, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China
Synopsis
Punctate white matter lesions (PWMLs) are common in the preterm. The mild PWMLs may result in cognitive impairments and lesion location is closely associated with neurodevelopmental outcomes. Accurate assessment of lesions location on qualitative MRI is difficult; therefore, this study aims to investigate the lesion-symptom relationship between locations of mild PWMLs and cognitive functioning in preterm infants at a corrected age of 3-6 months by diffusion tensor imaging. Lesion volume on IFOF_L is significantly larger in the cognitive delayed group than those in the normal group, and this is an independent factor (OR: 1.26) associated with the adverse cognitive development.
Introduction
White matter injury is common in preterm neonates, with the most common punctate white matter lesions (PWMLs) can be detected on conventional MRI as hyperintensity on T1WI and hypointenity on T2WI1. It is important to note that the lesions can gradually disappear along with time and are easily missed diagnosis, especially the mild subgroup. Previous studies have reported that mild PWMLs may mainly result in cognitive impairments and the lesion location is closely associated with the neurodevelopmental outcomes2, 3. However, accurate assessment of the lesions location on qualitative MRI images is difficult, and quantitative measurements may reveal more subtle alterations. Therefore, this study aims to investigate the lesion-symptom relationship between the locations of mild PWMLs and cognitive functioning in preterm infants at a corrected age (CA) of 3-6 months by diffusion tensor imaging.Methods
The local institutional review board approved this study and all the written informed consents were obtained from parents of the infants. Subjects Preterm infants (gestational age<37 weeks and postmenstrual age≤45 weeks) with evidence of mild PWML (diagnosed by conventional MRI: ≤10 lesions or 1 large lesion [diameter≥5mm]) were included. Bayley Scales of Infant Development II was used to evaluate the developmental outcomes at a CA of 3-6 months. According to the mental developmental index (MDI), the subjects with mild PWMLs were classified into normal group (MDI≥85) and delayed group (MDI<85). MRI Protocols All MR examinations were performed using a 3T scanner (Signa HDxt, GE Healthcare, Milwaukee, Wisconsin) with an 8-channel head coil. The scanning parameters of DTI sequence were as follows: 30 gradient directions; the number of excitations=1; b values=0 and 600s/mm2; TR/TE=11000/69.5ms; matrix size=128×128; slice thickness=2.5mm with no gap and FOV=180mm. Data and statistical analysis Tractography atlas for infants was obtained by using the registration between local infants and the JHU template. Twenty regions of interest were selected based on the labels, including commissural, association and projection fibers. After manual segmentation of the PWMLs on T1WI, the spatial relationships between lesion volume and the fasciculus were analyzed based on the individual level, and the lesion volumes on each fiber were calculated. Wilcoxon signed-rank tests were used to assess between group differences in demographics and neurodevelopmental outcomes, which were not normally distributed. The classification variables of the information were evaluated using Chi-square tests. Correlation between the lesion volume and MDI was performed using spearman partial correlation after controlling the postmenstrual age. Significantly different variables between two groups were analyzed in binary logistic regression to identify the factors that were associated with the cognitive outcome. Tests were considered significant at P<0.05.Results
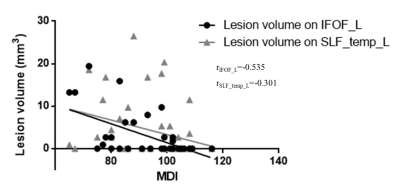
A total of 46 preterm infants with mild PWMLs were enrolled. Thirty-six and 10 subjects were classified into normal and delayed group, respectively. No significant differences in demographics and incidence of psychomotor development index (PDI) delay (4 subjects in each group) were found between the two groups (Table 1). Compared with normal group, the lesion volume on SCC, IFOF_L, UF_L and SLF_temp_L were significantly larger in delayed group than those in normal group (P<0.05, Figure 1). The lesion volume on IFOF_L (r=-0.535, P<0.001), SLF_temp_L (r=-0.301, P=0.044) was negatively correlated with MDI (Figure 2). Binary logistic regression revealed that the lesion volume on IFOF_L (OR: 1.26 [CI: 1.05-1.51], P=0.011) was an independent factor related to the cognitive score.Discussion
This study quantitatively characterized the lesion-symptom relationship in preterm infants with mild PWMLs, and the lesion volume on IFOF_L was an independent factor related to the adverse cognition outcome. The cognition of infant at 3-6 months is in the sensorimotor stage, which gathers and process cognitively salient information predominantly through auditory and visual means4. According to the parieto-frontal integration theory of intelligence, these basic sensory/perceptual are first fed forward to the parietal lobe, and further interacts with frontal regions to solute a given problem[4]. As a major long association fasciculus, IFOF connects occipital cortex, temporobasal areas, and superior parietal lobe to the frontal lobe5. The PWMLs located on this fasciculus may disturb the important pathways of facilitate rapid and error-free transmission of cognitively related information. Additionally, IFOF_L is closely associated with ventral-stream pathway of semantic processing and visual conceptualization for the subjects exposed to the Chinese6. The impairment of IFOF_L caused by PWMLs during the critical developmental period may be related to their future language development.Conclusion
Left IFOF is the key anatomical location of cognitive development delay in preterm infants with mild PWMLs at a CA of 3-6 months.Acknowledgements
This study was supported by the National Natural Science Foundation of China (No. 81971581, 81771810, 81471631 and 51706178), the 2011 New Century Excellent Talent Support Plan of the Ministry of Education, China (NCET-11-0438) and the Clinical Research Award of the First Affiliated Hospital of Xi’an Jiaotong University (No. XJTU1AF-CRF-2015-004).References
1.Wagenaar N, Chau V, Groenendaal F, et al. Clinical Risk Factors for Punctate White Matter Lesions on Early Magnetic Resonance Imaging in Preterm Newborns [J]. The Journal of pediatrics, 2017, 182(34-40.e1.
2. Guo T, Duerden EG, Adams E, et al. Quantitative assessment of white matter injury in preterm neonates: Association with outcomes [J]. Neurology, 2017, 88(7): 614-22.
3. Cayam-Rand D, Guo T, Grunau RE, et al. Predicting developmental outcomes in preterm infants: A simple white matter injury imaging rule [J]. Neurology, 2019, 93(13): e1231-e40.
4. Jung RE, Haier RJ. The Parieto-Frontal Integration Theory (P-FIT) of intelligence: converging neuroimaging evidence [J]. The Behavioral and brain sciences, 2007, 30(2): 135-54; discussion 54-87.
5. Wu Y, Sun D, Wang Y, et al. Subcomponents and Connectivity of the Inferior Fronto-Occipital Fasciculus Revealed by Diffusion Spectrum Imaging Fiber Tracking [J]. Frontiers in neuroanatomy, 2016, 10(88.
6. Ge J, Peng G, Lyu B, et al. Cross-language differences in the brain network subserving intelligible speech [J]. Proceedings of the National Academy of Sciences of the United States of America, 2015, 112(10): 2972-7.