4622
High-resolution MRI of retinoblastoma achieved by the dedicated pediatric coil at 3T1Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, China, shenzhen, China, 2Department of Radiology, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China,, Shanghai, China, 3Shanghai United Imaging, Shanghai, China, Shanghai, China, 4Department of Biomedical Engineering, State University of New York at Buffalo, NY, United States., Buffalo, NY, United States, 5Lauterbur Imaging Research Center, Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, China, shenzhen, China
Synopsis
High resolution MRI has become a very useful diagnostic tool in evaluation children with retinoblastoma. In this paper, higher spatial resolution images of retinoblastoma in 3T MRI were acquired by using the dedicated pediatric coil with optimized imaging protocol. 8 examinations in this study were analyzed and assessed. The results show that all were achieved the good image quality, which is very significance for the accurate diagnosis in retinoblastoma and evaluation of therapeutic effect in clinically.
Introduction
Retinoblastoma is the most common primary malignant tumor of the retina in child. Magnetic resonance imaging (MRI) as a tool for initial imaging and follow-up before treatment, has played a critical role in the assignment diagnosing, staging, and follow-up of intraocular retinoblastoma in children due to its high tissue contrast 1. The detection and exclusion of risk factors for metastasis is critical for the appropriate treatment for retinoblastoma in children 2. With the increasing use of eye-saving treatment strategies, more children are treated with non-invasive diagnostic tool without histopathological validation of the diagnosis 3. The potential for fast, high-resolution imaging using the pediatric coils has been demonstrated in the previous study4. In this study, we proposed an optimized protocol in retinoblastoma imaging for the dedicated pediatric coil. 8 examinations were analyzed and assessed. All of the exams achieved the good image quality, which has the clinically significance for the accurate diagnosis and evaluation of therapeutic treatment of retinoblastoma.Method
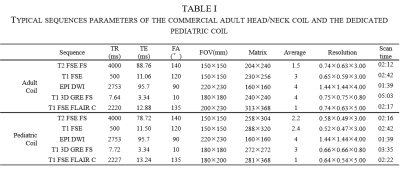
With the Ethics Committee of Xinhua Hospital Affiliations to shanghai Jiao Tong University school of Medicine approval and informed patient consent, we evaluated MRI scans from 8 retinoblastoma patients between August to October 2019 from the Xinhua Hospital Affiliations to shanghai Jiao Tong University. All were scanned on a 3T MRI system (UMR 770, Shanghai United Imaging Healthcare, Shanghai, China) in the dedicated pediatric coil with an optimized imaging protocol.All examinations were scanned under general sedation to ensure sufficient reduction of motion artifacts. As contrast agent we used an intravenous injection of 0.1 mmol/kg of gadoteric acid. The detailed imaging sequences were shown in Table I. High spatial resolution images of two retinoblastoma patients were acquired from the adult head/neck coil and the dedicated pediatric coil, respectively. The images of the typical sequences were compared. Additionally, routine brain imaging was performed on T1 weighted fluid attenuated inversion recovery contrast-enhancement fast spin echo in all examinations to exclude trilateral retinoblastoma at the time of diagnosis.
All image analysis was performed by two radiologists in rich experience and assessed the quality of the images independently on a scale from nondiagnostic (score=1), limited (score=2), average (score=3), good (score=4), excellent (score=5) in three aspects including tissue contrast, anatomical clarity and image uniformity.
Result
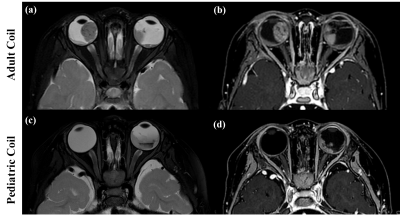
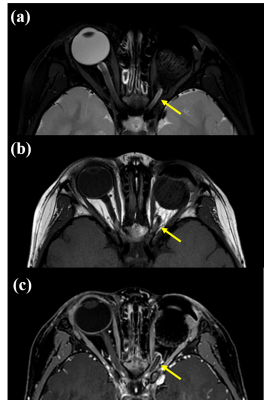
Representative images of two patients from the two coils were shown in Fig.1. In the T2-weighted fast spin echo with fat-saturation images, as shown in the Fig.1(a) and (c), The higher resolution 0.29 mm × 0.25 mm after 2-fold interpolation in 2 min 16 seconds were achieved by the pediatric coil, it can support the implementation of the parallel imaging reconstruction in 1.8-fold acceleration with high SNR. While in the adult head/neck coil, the resolution 0.37 mm × 0.31mm after 2-fold interpolation in 2 min 12 seconds can be achieved, full encoding was needed to maintain the image quality. The Fig1. (b) and (d) shows the 3D T1-weighted gradient echo sequence with fat-saturation images. Better details are displayed in the images acquired by the pediatric coil. Sharper of the optic nerve boundary can be seen and the shape is more realistic and more visible than the surrounding structure. With a little shorter of echo time, the shape of tissue and muscle in the inner wall of the eye frame can be more clearly observed. Representative images of a 2-year-old retinoblastoma patient with excision of left eye are shown in Fig. 2. No thickening and enhancement can be observed more accurately in the optic nerve stump in Fig.2 (c) and no signs of tumor recurrence were found in the left eye frame. The mean score for overall image quality of the 10 examinations was 4.9, 4.95 and 4.95 in tissue contrast, anatomical clarity and image uniformity, respectively. All of the exams achieved the good image quality (score=4 and 5).Conclusion/discussion
The higher resolution images of retinoblastoma patients were successfully acquired by using the dedicated pediatric coil with the optimized imaging protocol in this work. The results of image quality evaluation in the clinical 8 examinations demonstrated the advantages. The ability of MRI to detect metastatic risk factors and clinical diagnosing of retinoblastoma can be improved with higher resolution.Acknowledgements
This work was supported in part by NSFC under Grant No. 61571433, 61801466, 81627901, 81527901; Grant No. 2017YFC0109000; Guangdong Province grants 2014A030312006, and 2014B030301013; Youth Innovation Promotion Association of CAS No. 2017415; and city grants JCYJ20170413161314734.References
1. M. C. De Jong, et, al, “The potential of 3T high-resolution magnetic resonance imaging for diagnosis, staging, and follow-up of retinoblastoma,” Survey of Ophthalmology, vol.60, no.4, pp:346-355. 2015
2. S. Sirin, et.al. “High-resolution MRI using orbit surface coils for the evaluation of metastatic risk factors in 143 children with retinoblastoma,” Neuroradiology, vol.57,pp:805-814.2015
3. S. Chen, et, al. “The value of MRI in evaluating the efficacy and complications with the treatment of intra-arterial chemotherapy for retinoblastoma,” Oncotarget. vol.8, no.24, pp:38413-38425,2017,
4. Y. Li, et.al. “A 24-channel head and spine array for 3T pediatric MRI under 3-year-old,” 27th ISMRM
Figures