4594
Prediction of spastic cerebral palsy based on radiographic feature in children with periventricular leukomalacia1The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China, 2The First Affiliated Hospital of Henan University of traditional Chinese Medicine, Zhengzhou, China, 3Xi’an Children Hospital, Xi’an, China, 4GE Healthcare, Peking, China, 5The First Affiliated Hospital of Xi’an Jiaotong University, Zhengzhou, China
Synopsis
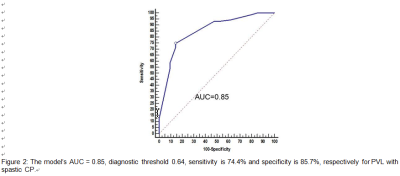
Early identification of classification of cerebral palsy (CP) in children with periventricular leukomalacia (PVL) is crucial for specific rehabilitation treatment and improving the quality of life. In this study, we retrospectively analyzed the baseline clinical data and visually assessed PVL-associated MR signs in children with CP, found that T2WI abnormal hyperintensity in body of lateral ventricle, posterior limb of internal capsule (PLIC), lenticular nucleus and white matter volume reduction were independent predictors of spastic CP. Results indicated that the area under receiver operating characteristic curve of multivariate regression model was 0.85, sensitivity and specificity for this model were 74.4% and 85.7%, respectively.
Synopsis
Early identification of classification of cerebral palsy (CP) in children with periventricular leukomalacia (PVL) is crucial for specific rehabilitation treatment and improving the quality of life. In this study, we retrospectively analyzed the baseline clinical data and visually assessed PVL-associated MR signs in children with CP, found that T2WI abnormal hyperintensity in body of lateral ventricle, posterior limb of internal capsule (PLIC), lenticular nucleus and white matter volume reduction were independent predictors of spastic CP. Results indicated that the area under receiver operating characteristic curve of multivariate regression model was 0.85, sensitivity and specificity for this model were 74.4% and 85.7%, respectively.Introduction
Cerebral palsy (CP) is the main cause of persistent motor impairment and disability with children1. Periventricular leukomalacia (PVL) is a sequelae of brain injury caused by ischemia and hypoxia in premature infants2. It is also one of the main causes of CP3. In PVL children with CP, spastic CP is the most common type, followed by mixed type, and dyskinetic is rare. The CP guidelines4 proposed that it is difficult to determine the type of CP before the age of 2 years. Previous studies5,6 reported the various PVL-associated MR features; among them, some were suggested as potential biomarkers in type of CP prediction. However, the responsible lesion and pathogenesis of CP injury caused by PVL unclear, a clinically-practical prediction method remains absent. To address such issue, we visually assessed series of PVL-associated MR signs and explored radiographic feature in predicting spastic CP.Methods
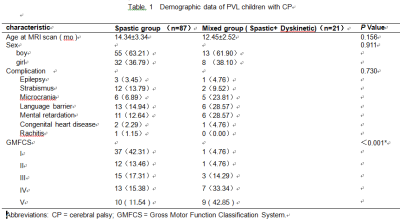
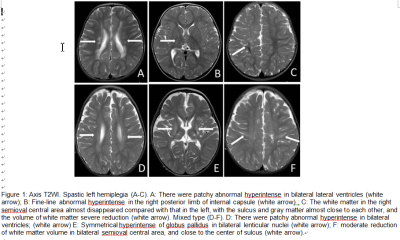
From April 2013 to April 2019, 111 PVL children with CP aged less than 2 yr (boy/girl, 69/42; age, 4~23 mo) diagnosed by the First Affiliated Hospital of Henan University of Chinese Medicine were enrolled. Among them, one case of dyskinetic type, hypotonic type and ataxia type were excluded and eventually divided into spastic CP group (n=87) and mixed (Spastic+ Dyskinetic) CP group (n=21). MR signs (T2 abnormal hyperintensity in body of lateral ventricle, posterior limb of internal capsule (PLIC), lenticular nucleus and white matter volume reduction) were assessed by a visually scoring method, and were evaluated for predicting the type of CP based on a binary logistic regression (Figure 1). The overall ability of predictive model to discriminate between spastic CP and mixed CP was analyzed using a binary receiver operating characteristic (ROC) regression analysis and quantified using the areas under the ROC curves (AUC). P<0.05 indicated that the difference was statistically significant. Analyses were performed with software SPSS 22.0 for IBM (SPSS Inc. Chicago, IL, USA), MedcCalc (ver 13.0.0.0, bvba).Results
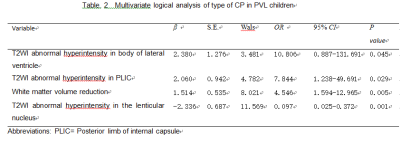
There were 87 of 108 PVL children with spastic CP, the incidence was 80.55%. Demographic, clinical variables for the study cohort are depicted in Table 1. No significant difference was found between spastic CP and mixed CP groups in terms of sex and age. Multivariate logistic regression analysis showed that T2WI abnormal hyperintensity in body of lateral ventricle (OR=10.81, 95% CI 0.89-131.69), PLIC (OR=7.84, 95%CI 1.24-49.69), lenticular nucleus (OR=0.97, 95% CI 0.03-0.37) and white matter volume reduction (OR=4.55, 95%CI1.59-12.97) were independent predictors of spastic CP. The lenticular nucleus was negatively correlated with spastic CP , when abnormal hyperintensity appears in lenticular nucleus, it is more likely to be mixed CP. (Table 2, Figure 1). The regression equation is as follows:Logit (P / spastic type) = - 7.746 + 2.380 ×T2WI abnormal hyperintensity in body of lateral ventricle + 2.060 ×T2WI abnormal hyperintensity in posterior limb of the internal capsule + 1.541 ×white matter volume reduction-2.336 ×T2WI abnormal hyperintensity in the lenticular nucleusResults indicated that the area under receiver operating characteristic curve of multivariate regression model was 0.85, sensitivity and specificity for this model were 74.4% and 85.7%, respectively. (Figure 2).Discussion
In this study, we developed a practical MR modle to predict the spastic CP in PVL children before 2 years old by assessing several MR signs. The role of MRI in predicting CP has been previously studied7,8. But the prediction type of CP has not been reported. We found that T2WI abnormal hyperintensity in body of lateral ventricle, posterior limb of internal capsule (PLIC), lenticular nucleus and white matter volume reduction presented higher ability in risk prediction of spastic CP. Among these, body of lateral ventricle, PLIC located in the centralized walking area of corticospinal tract. In particular, lesions in body of lateral ventricle and PLIC have been demonstrated to show close link with spastic CP. In this regard, abnormal MR findings of PVL in these regions may be considered as risk predictors. The synergism of the above factors leads to the decrease of the number of nerve fibers and the interruption of projections, which leads to the abnormality of nerve connections and the influence of nerve information transmission pathway, leads to the occurrence of motor dysfunction and CP. Besides, severe PVL also involved lenticular nucleus, especially the globus pallidus. Lenticular nucleus plays critical roles in inhibits the involuntary and hinders the coordinated movement9. Among them, the injury of globus pallidus is closely related to gross motor function10.Conclusion
The type of CP in PVL children can be predicted early based on the above independent predictors, which can guiding significance for early targeted rehabilitation treatment.Acknowledgements
This work was supported by the National Key Research and Development Program of China (2016YFC0100300), National Natural Science Foundation of China (No.81171317, 81471631), and the 2011 New Century Excellent Talent Support Plan of the Ministry of Education, China (NCET-11-0438).References
1. Martinez-Biarge M, Diez-Sebastian J, Kapellou O, et al. Predicting motor outcome and death in term hypoxic-ischemic encephalopathy[J]. Neurology 2011, 76(24):2055-2061.
2. Imamura T, Ariga H, Kaneko M, et al. Neurodevelopmental outcomes of children with periventricular leukomalacia. Pediatrics and Neonatology[J]. 2013; 54(6):367-72.
3. Herskind A,Greisen G,Nielsen JB. Early identification and interventionin cerebral palsy[J]. Dev Med Child Neurol,2015,57(1):29-36.
4. Novak I, Morgan C, Adde L, et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment[J]. JAMA Pediatr. 2017 Sep 1;171(9):897-907.
5. Palisano R, Rosenbaum P, Walter S, Russell D, et al. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997;39(4):214-23.
6. George JM, Boyd RN, Colditz PB, et al.PPREMO: a prospective cohort study of preterm infant brain structure and function to predict neurodevelopmental outcome. BMC Pediatr. 2015 ;16;15:123.
7. Woodward LJ, Anderson PJ, Austin NC, Howard K, et al. Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N Engl J Med 2006;355(7):685-94.
8. Slaughter LA, Bonfante-Mejia E, Hintz SR,et al. Early Conventional MRI for Prediction of Neurodevelopmental Impairment in Extremely-Low-Birth-Weight Infants. Neonatology 2016;110(1):47-54.
9. Martinez-Biarge M, Diez-Sebastian J, Kapellou O ,et al. Predictingmotor outcome and death in term hypoxic-ischemic encephalopathy[J]. Neurology,2011,76(24):2055-2261.
10. de Vries LS1, van Haastert IC, Benders MJ, et al. Cerebral palsy cannot be predicted by neonatal brain imaging[J]. Semin Fetal Neonatal Med 2011,16(5):279-287.