4583
Assisted vaginal delivery increases the risk of punctate white matter lesions in neonatal brain found by MRI1the First Afliated Hospital of Xi'an Jiaotong University, Xi'an, China
Synopsis
Punctate white matter lesion (PWML) was the common abnormal findings by MRI in neonates, which might predict poor motor and cognitive outcomes. Assisted vaginal delivery (AVD) increased brain injury. But the association between AVD and PWML is not clear. This study showed the mode of delivery is associated with PWML. AVD markedly increased the risk of PWML compared with cesarean delivery, especially vacuum extraction with cesarean section as a reference. The incidence of II and III-IV grade PWML of neonates with AVD was much higher than that with cesarean section.
Introduction
White matter injury (WMI) was the common abnormal findings by MRI in neonates, especially punctate white matter lesion (PWML)1,2,which was ccounted for 20-30%1-3. The incidence of PWML is about 20-30%1-3, which might predict poor motor and cognitive outcomes4-6,16. The process of delivery may cause brain injury including PWML. Assisted vaginal delivery (AVD) is an important method to expedite vaginal delivery as soon as possible in emergency situations. AVD increased the prevalence of cerebral hemorrhage7,8. The association between AVD and PWML is not clear.Materials and Methods
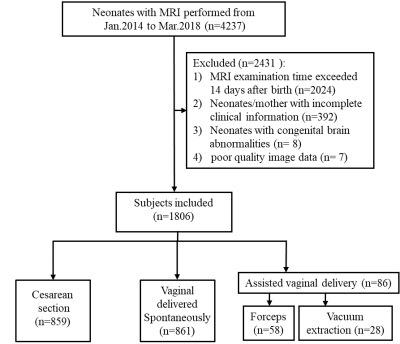
This was an observational cohort study included neonatal data from 6 clinical centers from Jan.2014 to Mar.2018 (First Affiliated Hospital of Xi'an Jiaotong University, Northwest Women and Children's Hospital, Xi'an Children's Hospital, Xi’an Gaoxin Hospital, Shaanxi Provincial People's Hospital, Ankang City Center Hospital, Baoji Central Hospital, Affiliated Hospital of Shanxi Medical University and General Hospital of Ningxia Medical University ). This study has been approved by the institutional review board of the First Affiliated Hospital of Xi’an Jiaotong University in Xi’an, Shaanxi, China. This study is a part of clinical trial that has been registered with the Clinical Trials Registry (NCT02637817). Informed consent was signed by the parents or legal guardian of each baby. Neonates who had undergone magnetic resonance imaging (MRI) examination and related clinical information were included. MRI was used to diagnose and classify PWML. Final multivariable was used to analyze the association of mode of delivery with PWML. Primary outcome was the diagnosis of PWML by MRI. Logistic regression was used to evaluate the association of mode of delivery with PWML adjusted for potentially perinatal and postnatal confounding variables. Then the grading logistic regression of head circumference and primipara was carried out.Results
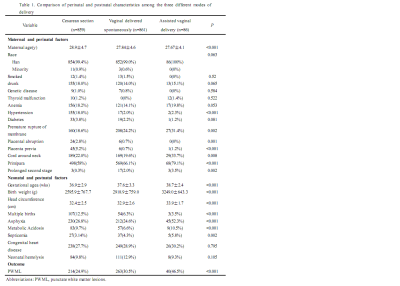
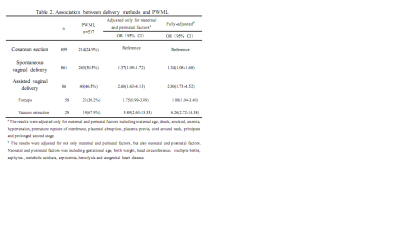
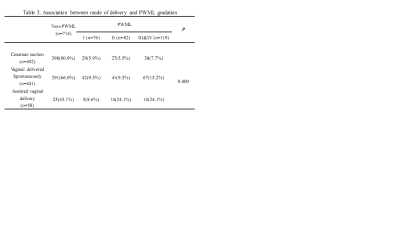
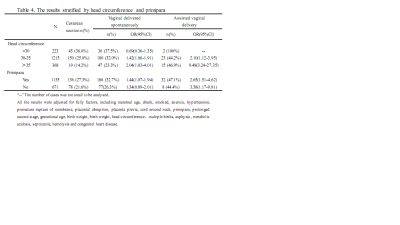
This study collected 4237 neonates and 1806 neonates (762 male) in the final cohort, 517 (28.6%) were diagnosed with PWML by MRI. The incidence of PWML in cesarean section, normal vaginal delivery and assisted vaginal delivery (AVD) group was 24.9%, 30.5% and 46.5%, respectively. Neonates with spontaneous vaginal delivery marginally increased odds of PWML (odds ratio [OR] 1.34, 95% CI 1.08-1.68) adjusted for perinatal and postnatal variables with cesarean section as a reference. AVD group had a higher odd (OR 2.80; 95% CI 1.73-4.52) of PWML. Forceps (OR 1.88, 95% CI 1.04-3.40) and vacuum extraction (OR 6.25, 95% CI 2.72-14.38) increased the risk of PWML obviously. According to clinical experience and previous reports, head circumference and primipara have important influence on the choice of delivery mode. So the further grading analysis of head circumference and primipara was carried out. The results showed that no matter normal or AVD, if head circumference >30cm, the larger the head circumference, the higher the risk of PWML. The incidence of PWML increased in primipara group with normal vaginal delivery, but it did not occur in multipara.Discussion
Based on our results it was firstly suggested that the mode of delivery can affect the risk of PWML. The results showed that vaginal delivery spontaneously slightly increases the odds of PWML, while AVD can significantly increase the odds, especially vacuum extraction with cesarean section as a reference. The incidence of II and III-IV grade PWML of neonates with AVD was much higher than that with cesarean section. The results of stratified analysis demonstrated that the larger the neonatal head, the higher the risk of PWML no matter natural vaginal delivery or AVD. In the population of multipara, natural vaginal delivery did not increase the risk of PWML, but AVD still significantly increases the odds ratio of PWML. The researchers believed that the occurrence of PWML may be related to the injury of immature oligodendrocytes9, which were very sensitive to ischemia and hypoxia and prone to injury10. We speculated that long periods of intermittent uterine contractions during vaginal delivery may lead a potential hypoxia environment for the fetus, which may increase risk of PWML. Neonates who experience AVD may have a greater degree of hypoxia. Because most mothers who need AVD were exhausted or had a prolonged second stage of labor11, the supply of oxygen to the fetus may be reduced and keep the fetus in an anoxic environment for longer11,12. It was reported that neonates with AVD had a lower fetal arterial oxygen saturation levels than that of neonates with natural vaginal delivery13. Furthermore, neonates with AVD experienced not only the extrusion of the birth canal, but also the direct extrusion of vacuum extraction or forcep. This double compression made the fetal head more vulnerable. It has been confirmed that AVD increased the prevalence of cerebral hemorrhage compared with natural vaginal delivery14,15.Conclusion
The mode of delivery is associated with PWML. AVD markedly increased the risk of PWML compared with cesarean delivery.Acknowledgements
noReferences
1. Kersbergen KJ, Benders MJ, Groenendaal F, et al. Different patterns of punctate white matter lesions in serially scanned preterm infants. PLoS One. 2014;9(10):e108904.
2. de Bruine FT, van den Berg-Huysmans AA, Leijser LM, et al. Clinical implications of MR imaging findings in the white matter in very preterm infants: a 2-year follow-up study. Radiology. 2011;261(3):899-906. 3. Wagenaar N, Chau V, Groenendaal F, et al. Clinical Risk Factors for Punctate White Matter Lesions on Early Magnetic Resonance Imaging in Preterm Newborns. J Pediatr. 2017;182:34-40 e31.
4. Zhang Y, Rauscher A, Kames C, Weber AM. Quantitative Analysis of Punctate White Matter Lesions in Neonates Using Quantitative Susceptibility Mapping and R2* Relaxation. AJNR Am J Neuroradiol. 2019;40(7):1221-1226.
5. Guo T, Duerden EG, Adams E, et al. Quantitative assessment of white matter injury in preterm neonates: Association with outcomes. Neurology. 2017;88(7):614-622.
6. Bassi L, Chew A, Merchant N, et al. Diffusion tensor imaging in preterm infants with punctate white matter lesions. Pediatr Res. 2011;69(6):561-566.
7. Salman L, Aviram A, Krispin E, Wiznitzer A, Chen R, Gabbay-Benziv R. Adverse neonatal and maternal outcome following vacuum-assisted vaginal delivery: does indication matter? Arch Gynecol Obstet. 2017;295(5):1145-1150.
8. Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341(23):1709-1714.
9. Ramenghi LA, Fumagalli M, Righini A, et al. Magnetic resonance imaging assessment of brain maturation in preterm neonates with punctate white matter lesions. Neuroradiology. 2007;49(2):161-167. 10. Rathnasamy G, Murugan M, Ling EA, Kaur C. Hypoxia-Induced Iron Accumulation in Oligodendrocytes Mediates Apoptosis by Eliciting Endoplasmic Reticulum Stress. Mol Neurobiol. 2016;53(7):4713-4727
11. Dietz HP. Obstetric Forceps: A Species on the Brink of Extinction andForceps, Simulation, and Social Media andSimulation Training for Forceps-Assisted Vaginal Delivery and Rates of Maternal Perineal Trauma. Obstet Gynecol. 2016;128(6):1447-1448.
12. Polkowski M, Kuehnle E, Schippert C, Kundu S, Hillemanns P, Staboulidou I. Neonatal and Maternal Short-Term Outcome Parameters in Instrument-Assisted Vaginal Delivery Compared to Second Stage Cesarean Section in Labour: A Retrospective 11-Year Analysis. Gynecol Obstet Invest. 2018;83(1):90-98. 13. Salamalekis E, Vitoratos N, Kassanos D, et al. The influence of vacuum extractor on fetal oxygenation and newborn status. Arch Gynecol Obstet. 2005;271(2):119-122.
14. Salman L, Aviram A, Krispin E, Wiznitzer A, Chen R, Gabbay-Benziv R. Adverse neonatal and maternal outcome following vacuum-assisted vaginal delivery: does indication matter? Arch Gynecol Obstet. 2017;295(5):1145-1150.
15. Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341(23):1709-1714.
16. Nguyen ALA, Ding Y, Suffren S, Londono I, Luck D, Lodygensky GA. The brain’s kryptonite: Overview of punctate white matter lesions in neonates. International Journal of Developmental Neuroscience. 2019
Figures