4565
Breast MRI combined with clinicopathologic characteristics for Preoperative Prediction of Axillary Lymph Node Metastasis in Breast Cancer1Radiology, Cancer Hospital Chinese Academy of Medical Sciences, Beijing, China, 2GE Healthcare, MR Research China, Beijing, Beijing, China, 3Cancer Hospital Chinese Academy of Medical Sciences, Beijing, China
Synopsis
Accurate identification of axillary lymph node(ALN) involvement in patients with breast cancer is crucial for prognosis and treatment strategy decisions. We developed a clinical model based on breast MR imaging and clinicopathologic characteristics to predict ALN metastasis. Our findings suggest that the clinicopathological features of breast tumor are highly correlated with axillary lymph node metastasis. It can be used to assist clinicians to predict LN metastasis non-invasively.
Introduction
Axillary lymph node (ALN) status is an important prognostic factor for overall breast cancer survival. The number of axillary lymph node metastases is closely related to the risk of distant metastasis1. Accurate identification of axillary lymph node involvement in patients with breast cancer is crucial for prognosis and treatment strategy decisions. Axillary lymph node dissection (ALND) is currently the standard procedure for determining ALN status. Sentinel lymph node biopsy was used to determine whether axillary lymph node dissection was needed, which is invasive2. Image based non-invasive predictors of axillary lymph nodes are highly desirable, and currently face challenges. Traditional imaging examinations have limited value for evaluating axillary LNs status. Moreover, it is difficult to match the LNs that have been biopsied or dissected was the LNs imaged on traditional imaging. The aim of this study was to explore the MR imaging features and clinicopathologic characteristics of breast tumor in correlation with axillary lymph node metastasis in breast cancer patients.Method
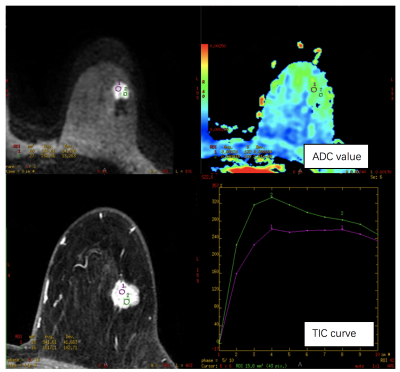
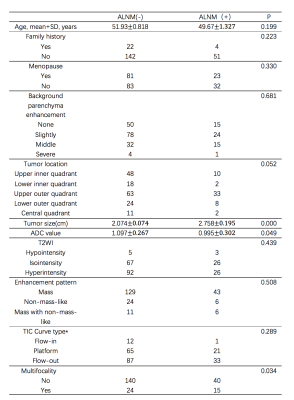
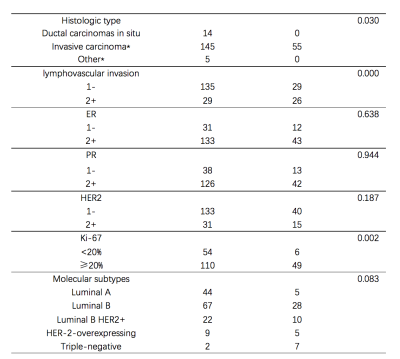
Patients with breast cancer confirmed by surgery and pathology were retrospectively reviewed at our institution between January 2016 to December 2016. All patients underwent MR examination before operation, and there were complete data of routine pathology, immunohistochemistry and axillary lymph node pathology after operation. The clinicopathological and MRI features of the primary breast cancer lesions were determined. The MR image characters including: tumor size, ADC value, enhancement pattern, TIC Curve type, multifocality (Figure 1). The clinicopathological characters including: LN status, histological tumor type, HER2, ER, PR, KI-67 levels, lymphovascular invasion, and molecular subtypes. According to the postoperative pathological results, the patients were divided into axillary lymph node metastasis (ALNM (+)) and non-metastasis lymph node group (ALNM (-)). The association between LN metastasis and conventional clinical risk factors was assessed using univariate analyses. Multivariate logistic regression analysis was performed to identify independent factors associated with lymph node status among the variables showing statistical significance on univariate analysis (P<0.05).Results
219 breast cancer patients were enrolled. 55 patients (25.1%) had metastatic ALNs, while 164 (74.9%) had no ALN metastasis. The MRI manifestations and clinical information of ALNM(+) and ALNM(-) group were given in Table 1. The pathological characteristics of ALNM(-) and ALNM(+) group were given in Table 2. Statistical differences were found between LN-metastasis group and non-LN-metastasis group in tumor size, ADC value, multifocality, histological type, lymphovascular invasion and the level of Ki-67 in the univariate analyses. There were no statistical differences between LN-metastasis group and non-LN-metastasis group in age, enhancement pattern, TIC curve type, ER, PR, HER2 and Molecular subtypes. In multivariate analysis, tumor size, multifocality, lymphovascular invasion and the level of Ki-67 were still independent variables related to axillary lymph node metastasis.Discussion
MRI has advantages in displaying soft tissue, because of its multidirectional, multiparameters, and multifunctional imaging, thus it showed a sensitivity of 95% to 99% in various breast cancer examinations3.While, there are defects of MRI in displaying axillary lymph nodes affected by acquisition coil. Our results demonstrate that the clinicopathological features of breast tumor are highly correlated with axillary lymph node metastasis. We developed a clinical model based on breast MR imaging and clinicopathologic characteristics to predict LN metastasis and the performance is quite satisfactory. It can be used to assist clinicians to predict LN metastasis non-invasively.Conclusion
Preoperative MRI can effectively evaluate axillary lymph node metastasis of breast cancer. Tumor size, lymphatic invasion and Ki67 level are the most powerful independent predictors of axillary lymph node metastasis.Acknowledgements
No acknowledgement found.References
1. Kohrt H E, Olshen R A, Bermas H R, et al. New models and online calculator for predicting non-sentinel lymph node status in sentinel lymph node positive breast cancer patients. BMC Cancer, 2008, 8(1): 66-66.
2. Esposito E, Micco R D, Gentilini O D. Sentinel node biopsy in early breast cancer. A review on recent and ongoing randomized trials[J]. Breast, 2017, 36:14.
3. Telegrafo M, Rella L, Stabile Ianora AA, et al. Breast MRI background parenchymal enhancement (BPE) correlates with the risk of breast cancer. Magn Reson Imaging 2016;34:173.