4295
On the way to routine cardiac MRI at 7Tesla- using what we have1Department of Internal Medicine, University Hospital Wuerzburg, Wuerzburg, Germany, 2Chair of Cellular and Molecular Imaging, Comprehensive Heart Failure Centre (CHCF), University Hospital Wuerzburg, Wuerzburg, Germany
Synopsis
The establishment of human cardiac MRI in the setting of ultra highfield MRI puts high demands on hardware, sequences and handling of the examinees. Practical and safety relevant limitations are set for extensive modifications regarding hardware and sequence. As a consequence, human based factors play a paramount role in the success of a routinely used cardiac imaging study at 7T. We report our experiences from 71 volunteers with cardiac MRI scans with the aim to increase the understanding of the practical implementation of cardiac MRI and factors that influence and do not influence image quality in this specific setting.
Introduction
Cardiac MRI at Ultra Highfield MRI is both highly alluring and challenging, offering the promise of high resolution myocardial images on one side, technical pitfalls such as pronounced magnetic field inhomogeneities and sequence limitations on the other side1-3. Smaller cardiac studies have offered a glimpse on what we can expect and hope for under ideal conditions4-6. Larger studies without a focus on cardiac 7T MRI have demonstrated the general acceptance in those examined albeit side effects such as vertigo and nausea during positioning7,8. The path towards more routinely used cardiac MRI at 7T is currently still troublesome, as it still requires the definition of optimal radiofrequency coils, pulse sequences and clinical practices.Motivation
The clinical benchmark with regard to the usability of cardiac MRI at 7T is image quality. It ensures the usability of the images, be it for scientific or for diagnostic purposes. This, a sufficient diagnostic image quality is the prerequisite for larger clinically orientated studies. Not all factors that play a role for image quality are easily influencable or are not even known at this point where a wider basis of clinical studies is still missing. Understanding the current capabilities with existing commercially available 7T MRI systems in this setting thus becomes an important starting point for the future optimization cardiac 7T MRI radiofrequency coil and pulse sequence development, and general measurement setup.Materials and Methods
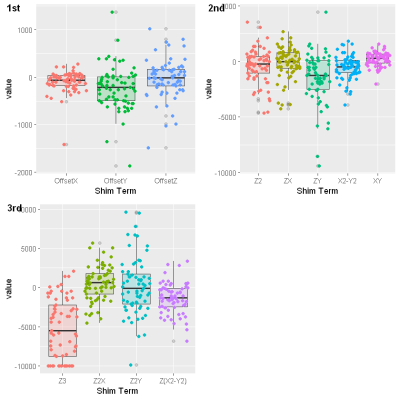
With permission of the local ethics committee, cardiac 7T MRI was performed in 71 healthy volunteers (mean age 32 years, weight 71 kg, 173 cm, BMI 23.6) using a latest technology 7T system with 3rd-order shim system (Magnetom Terra, Siemens Healthcare, Erlangen, Germany) between 2017 and 2019. All images were obtained using the vendor’s 1Tx/16Rx thorax coil. For retrospective cardiac triggering the scanner’s vector ECG and, as an alternative, the Easy ACT acoustic trigger system were used. The imaging protocol was part of the implementation and research work at the scanner, and among others consisted of survey, scouts, shim scans and functional CINE imaging in short and long axis views. For B0 shimming, a dual gradient-echo sequence, provided by the vendor was used. The shim volume covered the whole heart. For CINE imaging a gradient echo sequence (FOV 340 x 320 mm, slice thickness 6.0 mm, TE 3.56 ms, flip angle 12 - 47°, Grappa factor 2 or 3) was used. In 40 volunteers, a full short axis stack was obtained , which covered the complete ventricles with no interslice gap and 18 to 25 cardiac phases. The diagnostic imaging quality of all full short axis stacks were analyzed with a score focusing on artifact burden, noise and overall quality. Variation of image quality as a function of anterior and posterior coil positioning was analysed. Shim currents and ECG trigger quality was obtained from the DICOM image headers. Subjective acceptance of 7T MRI was analyzed, using a standardized questionnaire and compared with 42 volunteers, who had received a brain MRI at the same scanner.Results
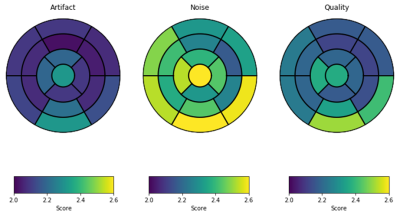
The diagnostic image quality and left ventricular function considered 680 left and 280 right ventricular segments. The mean left ventricular ejection fraction was 53%. In the left ventricle 14/680, in the right ventricle, 4/280 segments were non diagnostic. Overall image quality scores in the left and in the right ventricle were 2.25 and 2.47, respectively (Fig. 1). Acoustic and ECG triggering were used equally often. A switch in the trigger technique, however, proved to be a useful tool to improve image quality when the trigger system did not ensure reliable detection of the cardiac activity and occurred in 20% of all scans (Fig.2). The data from the shim coils covering first to third order of spherical harmonics are given in Fig3. Coil position and deviations from the optimal coil positioning did not significantly influence image quality. The subjective acceptance showed that the duration of the whole 7T exam (59%, mean value 3.02/10) was the most frequent, and paresthetic discomfort was rarest (22.5%, mean value 3.38/10) reason for discomfort. In addition, feelings of narrowness (38%, mean value 1.49/10), noise (40.8%, mean value 1.57/10) and vertigo during movement (26.8%, mean value 1.31) were noted. In comparison, during brain scans paresthetic discomfort (68,4%, mean value 3.45/10) was the most frequent and worst remark.Discussion
With only 18/960 analyzed segments being non diagnostic, the overall image quality allowed a diagnostic interpretation in all included volunteers. The data from coil positioning, shim currents and triggering showed that the commercially available equipment allows to produce stable results for cardiac CINE imaging. Both trigger options are currently helpful during the initial preparation of the subject. However, it currently appears helpful in some cases to have an triggering alternative. The vendor based 3rd-order B0 shimming shows satisfactory results, independently of suboptimal coil placement. The overall subjective acceptance for cardiac studies consistently was good. However, it has to be noted that the high end resolution images require further and in depths focus on factors others than the human based ones.Conclusion
On the way to routine cardiac MRI at 7T, the commercially available tools are already useful and robust, however, for highest resolution, further improvements are needed.Acknowledgements
Financial support was obtained from the German Ministry of Education and Research (BMBF) under grants: 01EO1004& 01EO1504.References
[1] Sievers et al.; (2011), Influence of the trigger technique on ventricular function measurement using 3-Tesla magnetic resonance imaging: comparison of ECG versus pulse wave triggering. Acta radiologica 2011;52:385-392.
[2] Stäb et al.; (2016): ECG Triggering in Ultra- High Field Cardiovascular MRI. Tomography.org, Vol.2, No. 3, 2016
[3] Frauenrath et al.; (2008): Acoustic cardiac triggering: a practical solution for synchronization and gating of cardiovascular magnetic resonance imaging at 7Tesla. Acta Acust United Ac (2008) 94:148–155
[4] Prothmann et al.; (2016) High Spatial Resolution Cardiovascular Magnetic Resonance at 7.0T in Patients with hypertrophic Cardiomyopathy- First Experiences: Lesson learned from 7T. Plos One 11(2):e0148066
[5] Knobelsdorff-Brenkenhoff et al.; (2013), Assessment of the right ventricle with cardiovascular magnetic resonance at 7 Tesla. JCMR 2013, 15:23
[6] Alfakih et al.; (2003), Normal human left and right ventricular dimensions for MRI as assessed by turbo gradient echo and steady-state free precession imaging sequences. J Magn Reson. Imaging. 2003; 17:323-29
[7] Rauschenberg et al.; (2013), Multicenter Study of subjective acceptance during magnetic resonance imaging an 7 and 9.4 T. Invest Radiol 2014;49:249-259
[8] Klix et al.; (2015), On the subjective acceptance during Cardiovascular Magnetic Resonance Imaging at 7.0Tesla. Plos One 10(1):e0117095
Figures