4270
Realistic MRI phantom for T2 and Quantitative Susceptibility Mapping1Biomedical Imaging Center, Pontificia Universidad Católica de Chile, Santiago, Chile, 2Millennium Nucleus for Cardiovascular Magnetic Resonance, Santiago, Chile, 3Department of Electrical Engineering, Pontificia Universidad Católica de Chile, Santiago, Chile, 4Faculty of Chemistry, Pontificia Universidad Católica de Chile, Santiago, Chile
Synopsis
In this
work, we present a realistic phantom made of a solid material that we
developed, which can mimic the human brain anatomy, including grey and white
matter. Our new material also allows us to modulate T2 and susceptibility
values by changing the ratios of a 4 component mix wich can result in T2 times
from 100ms to 250ms and susceptibility values close to the human brain.
Introduction
MRI phantoms are typically objects objected with simple geometrical patterns such as spheres and cylinders made of liquids or gels [1-4]. Although there are some phantoms capable of resembling human anatomy[5], they lack different contrast zones or require an artificial septa to keep the different liquid components apart. In this work we present an MRI phantom made of solid materials capable of resembling complex anatomical shapes (e.g. a brain), with multiple compartments, modulating T2 and susceptibility. Due to its solid configuration, it does not require intervening septa and provides several advantages, including, mechanical and temporal stability.Methodology
As a proof of concept, we built a two-compartment brain slice (Fig 1) made of a 4-component material: silicone, silicone thinner, polyether polymer, and graphite. Whereas the graphite is capable of modulating the magnetic susceptibility properties [6], the polymer is capable of modulating the T2 properties independently [7]. For the white matter we used a commercial 2-part silicone (90:10 mixing ratio). Silicone thinner was added to this mix (15% ratio of the total weight), forming what we call the base material. The final mix is composed of 20% of a polyether polymer, 2% of graphite powder and 78% of base material. This mix was poured into a white matter mold. The obtained piece was inserted into a grey matter mold and covered with a different mix, composed of 10% of silicone thinner, 0,01% of graphite and no extra polymer. The obtained phantom was characterized using a turbo spin echo (TR/TE/ΔTE=2000/30/25ms, 8 echoes) and a turbo gradient echo sequence (TR/TE/ΔTE=44/4.6/8.6ms, 5 echoes) in a Philips 1.5T Achieva scanner. We computed T2, T2*(using an in-house developed Matlab code) and QSM maps of the phantom using FANSI [8, 9].Results and discussion
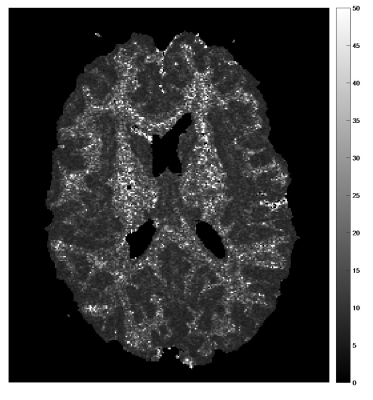
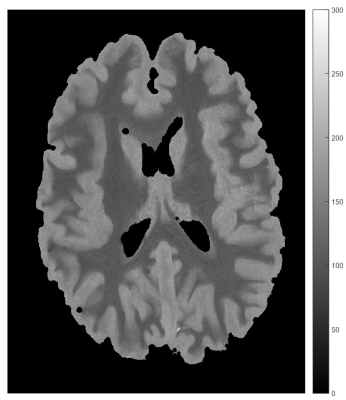
T2* values (Figure 2) were around 20-25ms for white matter and around 10-15ms for grey matter. In a previous work[7] we found that the amount of polymer can modify the T2 and T2* values of the obtained phantom, this behavior is still present adding graphite to the phantom.T2 (Figure 3)values were close to 100ms and 150ms for the white and grey matter, respectively.
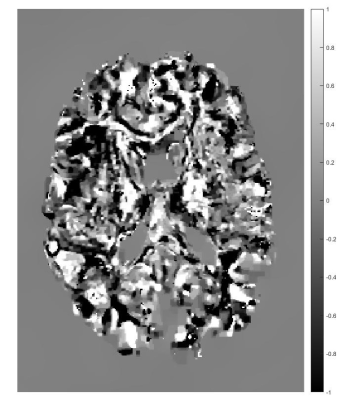
The susceptibility values of the resulting phantom (Figure 4) are not currently close to those of the human brain. Previous results (not shown) shows that when no graphite was added, the susceptibility was close to the human tisues, but the different material mixes where almost indistinguishable. More work must be donde in order to find the right amount of graphite or if there are any anisothopic effect in the phantom.
Acknowledgements
Grant funding Fondecyt 1191710, Anillo 190064, Millenium Science Initiative of the Ministry of Economy, Development and Tourism, grant Nucleus for Cardiovascular Magnetic Resonance.References
1. Gunter, J.L., et al., Measurement of MRI scanner performance with the ADNI phantom. Medical Physics, 2009. 36(6): p. 2193-2205.
2. Qiu, J., et al., Design of multi-function MR test phantom. Chin. J. Med. Imaging Technol, 2012. 28: p. 997-1000.
3. Keenan, K.E., et al., Design of a breast phantom for quantitative MRI. Journal of Magnetic Resonance Imaging, 2016: p. n/a-n/a.
4. Russek, S.E., et al. Characterization of NIST/ISMRM MRI system phantom. in Proc. Intl. Soc. Mag. Reson. Med. 2012.
5. Peerlings, J., et al., Characterizing geometrical accuracy in clinically optimised 7T and 3T magnetic resonance images for high-precision radiation treatment of brain tumours. Physics and Imaging in Radiation Oncology, 2019. 9: p. 35-42.
6. Chapa, M., et al. Development of a solid phantom for QSM and relaxometry applications. in 5th INTERNATIONAL WORKSHOP ON MRI PHASE CONTRAST & QUANTITATIVE SUSCEPTIBILITY MAPPING. 2019. Seoul, South Korea.
7. M. Chapa, H.V., C. Montalba, S. Uribe, M. Andia, F. Zacconi, C. Tejos. Solid material resembling human tissues:a white and gray matter brain phantom. in ISMRM 27th Annual Meeting & Exhibition. 2019. Palais des congrès de Montréal, 1001 Place Jean-Paul-Riopelle, Montréal, QC, Canada.
8. Bilgic, B., et al., Sparse methods for Quantitative Susceptibility Mapping. SPIE Optical Engineering + Applications. Vol. 9597. 2015: SPIE.
9. Milovic, C., et al., Fast nonlinear susceptibility inversion with variational regularization. Magnetic Resonance in Medicine, 2018. 80(2): p. 814-821.