4207
Acoustic Behavior of High Performance Imaging on a Head-only 0.5T Scanner with Asymmetric Gradients1Synaptive Medical, Toronto, ON, Canada
Synopsis
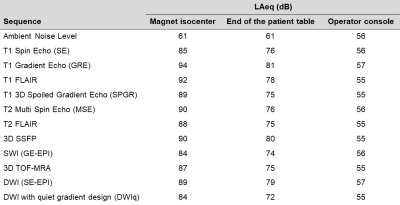
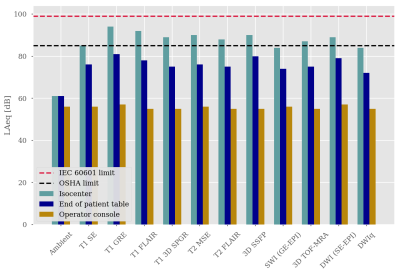
In this work the acoustic behavior of a 0.5T head-only scanner is demonstrated. Measurements of the A-weighted equivalent continuous sound level (LAeq) over a 10-second period were made for typical clinical protocols at three locations: magnet isocenter; within the magnet room but outside the magnet bore; and at the operator console – outside of the magnet room. The LAeq values varied between 84-94 dB, 74-81 dB, and 55-57 dB at the three measurement positions respectively. Notably, outside of the MR room, the LAeq levels were indistinguishable from ambient levels, suggesting minimal environmental acoustic impact near the magnet installation site.
Introduction
Modern MRI scanners can easily exceed peak acoustic energy values in excess of 100 dB [1,2]. This high sound pressure level exposure has been associated with temporary hearing loss [3-5] and increased patient anxiety [6]. Consequently, regulatory requirements restrict the peak acoustic energy of an MRI scanner to be below 140 dB and call for patient hearing protection when the A-weighted rms sound pressure level (LAeq) exceeds 99 db [7].In addition to patient safety issues, high sound levels can impact the environment around the MRI which raises concerns when installing a system outside of dedicated diagnostic imaging departments, such as in the ICU or Emergency Department. In this work, we demonstrate the acoustic performance of a small footprint, head-only 0.5T MR system with a high-performance gradient set which is more amenable for installation in non-conventional environments for point-of-care applications [8].
Methods
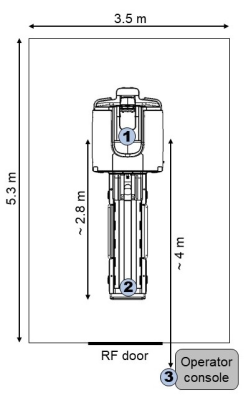
All scans were acquired on a head-specific 0.5T MR system equipped with a high performance gradient set with maximum gradient strength and slew rate of 100 mT/m and 400 T/m/s per axis respectively [8]. This MR system is stationed within a RF shielded room, constructed with ROCKWOOL SAFE’n’SOUND® (rockwool.com) soundproofing insulation, that is, the room wall consists of three layers: copper, soundproof insulation, and drywall. The door of the magnet room is a standard RF door without acoustic noise performance optimization.Recommended protocols of common clinical sequences were evaluated for their acoustic performance at 3 locations: magnet isocenter (inside the magnet bore); the foot of the patient bed (inside the magnet room but outside the magnet bore – approximately 2.8 m from isocenter); and the operator console (outside the RF shielded magnet room – approximately 4 m from isocenter) (Figure 1).
Measurements of the A-weighted, equivalent continuous sound level (LAeq) over a 10-second period were recorded for all sequences using a calibrated sound level meter with an MRI compatible microphone and input cable (Brüel & Kjær, Hand-held Analyzer Type 2250 with Microphone Unit Type 4188-L-001).
Lastly, the acoustic behavior of a diffusion-weighted imaging (DWI), echo-planar imaging (EPI), sequence with gradient waveforms adapted to minimize gradient acoustic resonances was also evaluated for its ability to reduce peak sound levels.
Results
Acoustic measurement results for all sequences and measurement locations is provided in Table 1 and visually displayed in Figure 2. The LAeq values varied between 84 – 94 dB, 74 – 81 dB, and 55-57 dB for all protocols at isocenter, the foot of the patient bed, and the operator console respectively.The DWI sequence with quiet gradient waveform design reduced the LAeq by 5-7 dB within the MR room compared to the standard sequence.
Discussion
Sound levels from MR systems have been shown to scale with field strength and with system parameters. Systems with higher gradient performance tend to have higher sound levels. Reported results for 0.5T systems with maximum gradient performance specifications (max amplitude and slew rate) of 16 mT/m and 25 T/m/s demonstrated maximum average sound levels of 93-95 dB [1]. Here, we present a head-only system with high performance gradients with similar maximum sound levels (94 dB) but with significantly higher gradient performance of 100 mT/m and 400 T/m/s.The Occupational Safety and Health Administration (OSHA) of the United States requires the implementation of a hearing conservation program (e.g. hearing protection) if the occupational noise exposure is at or above 85 dB averaged over 8 hours [9]. The maximum LAeq measured within the MR room at the end of the patient bed was 81 dB, significantly less than this limit. This allows for the possibility that point-of-care hospital staff could be present within the MR room without the need of hearing protection, which could significantly improve point-of-care imaging workflow.
At the operator console, outside of the MR room, the measured LAeq sound levels were indistinguishable from ambient noise levels, suggesting minimal environmental acoustic impact in the vicinity of its installation site.
A DWI, EPI-based, sequence with gradients designed to minimize the acoustic resonances of the system were able to reduce the modest acoustic levels by a further 5-7 dB. This gradient design scheme can easily be extended to other, noisier, sequences, without significant penalty in acquisition time.
Conclusion
A dedicated head-only 0.5T system is shown to have modest sound pressure levels which are comparable to low-field systems with significantly worse gradient performance. Intelligent gradient waveform design can further reduce acoustic levels. Measured sound levels external to the scanner room are indistinguishable from ambient levels and suggest the system would have minimal environmental acoustic impacts in areas where it is installed.Acknowledgements
No acknowledgement found.References
1. Price DL, De Wilde JP, Papadaki, AM, Curran JS, Kitney RI, “Investigation of Acoustic Noise on 15 MRI Scanners from 0.2 T to 3 T”, J Magn Reson Imaging, 2001, 13:288-293
2. Shellock FG, Ziarati M, Atkinson D, Chen DY, “Determination of gradient magnetic field-induced acoustic noise asscoated with the use of echo planara and three-dimensional, fast spin echo teqchniques”, J Magn Reson Imaging, 1998, 8(5), 1154-7
3. Brummett RE, Talbot JM, Charuhas P, “Potential hearing loss resulting from MR imaging”, Radiology, 1988, 169(2): 539-40
4. Jin C, Li H, Li X, Wang M, Liu C, Guo J, Yang J, “Temporary Hearing Threshold Shift in Healthy Volunteers with Hearing Protection Caused by Acoustic Noise Exposure during 3-T Multisequence MR Neuroimaging”, Radiology, 2018, 286(2): 602-8
5. Maryam Bahaloo, Mohammad Hossein Davari, Mohammad Sobhan, et al., “Hearing Thresholds Changes after MRI 1.5T of Head and Neck”, Radiology Research and Practice, vol. 2019, Article ID 8756579, 4 pages, 2019
6. Quirk MR, Letendre AJ, Ciottone RA, Lingley JF, “Anxiety in patients undergoing MR imaging”, Radiology, 1989, 170(2): 463-6
7. IEC 60601-2-33:2010, “Medical electrical equipment – Part 2-33: Particular requirements for the basic safety and essential performance of magnetic resonance equipment for medical diagnosis”, 2010, p. 17 & 28
8. Panther A, Thevathasen G, Connell IRO, Yao Y, Wiens CN, Curtis AT, Bindseil GA, Harris CT, Beatty PJ, Stainsby JA, Cunningham CH, Chronik BA, Piron C, “A Dedicated Head-Only MRI Scanner for Point-of-Care Imaging”. Proceedings of the 27th Annual Meeting of ISMRM. Montreal, Canada, 2019. Abstract 3679.
9. https://www.osha.gov/SLTC/noisehearingconservation
Figures