4190
3T RF Simulations of Pregnant Women and MR System Behaviour
Cecilia Possanzini1, Zhiyong Zhai2, and Paul Royston Harvey1
1MR R&D, Philips Healthcare, Best, Netherlands, 2Philips Healthcare, Gainesville, FL, United States
1MR R&D, Philips Healthcare, Best, Netherlands, 2Philips Healthcare, Gainesville, FL, United States
Synopsis
Scanning pregnant women in MRI systems operating at 3T has been a controversial issue with respect to RF exposure and RF field uniformity. The latter issue is solved by 3T parallel transmit systems. In this work, we demonstrate that, when scanning in normal operating mode, the simulated RF exposure increase is limited to an acceptable level when the real behaviour/constraints of the system are taken into account.
Introduction
Scanning pregnant women in MRI systems operating at 3T has been a controversial issue during recent years. IEC 60601-2-33 [1] prescribes scanning pregnant women in normal operating mode with respect to SAR levels. A frequently referenced publication [2] analysed the SAR and associated temperature increase for circularly polarized and various RF shimming modes at 3T and concluded that two-port RF shimming increases the RF exposure of the foetus resulting in a local increase in temperature in both foetus and mother. This work shows that, scanning with a 3T system in RF shimming mode, can be acceptable since, irrespective of the shim settings, the delivered SAR can be constrained by the system to 2 W/kg.Method
A 7-month pregnant woman was simulated at 3T using a two-port generic birdcage with a commercially available software (Sim4Life). The simulations targeted a constant B1+ (2.3µT) over the centre transversal slice at the isocenter for five different excitation settings: 1) circularly polarized mode (CP), 2) best homogeneity for mother, 3) best homogeneity for foetus, 4) worst case (WC, i.e. the highest) local SAR in mother, 5) worst case local SAR in foetus. In the last two cases, the simulation was also repeated targeting a constant Whole Body (WB) SAR of 2 W/kg (normal mode), 6) for the mother and 7) for the foetus, as in ref. [2]. The results are in agreement with ref. [2]. and the references therein. The simulated SAR values are then scaled to the real world system constrains: WB SAR of the mother in normal mode with a SAR overestimation factor of 1.5 for the mother WB SAR. Such a factor is used by all vendors [3].Results, discussion and conclusions
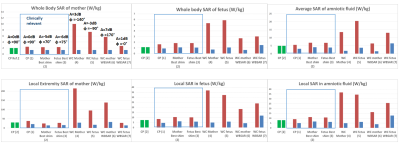
Figure 1 shows the SAR levels calculated for all scenarios described above (1-7). The SAR values obtained by simulations are the “unconstrained” values (red bars in figure 1), and the “constrained” values (blue bars), i.e. the SAR simulated values scaled down to meet the real world SAR constrains of the system. The CP mode SAR levels of ref. [2]. are displayed in green for comparison: Those levels are indicated in ref. [2]. as acceptable due to a moderate thermal exposure of mother and foetus (according to the thermal model proposed in the paper). Note that the B1+ reported in ref. [2]. for the CP case is lower (2.02mT) than the B1 targeted in this paper (2.3µT).The analysis of the RF shim settings reveals that some RF shimming modes are highly inefficient from a power perspective and they can require more RF power than the system can typically provide. The power efficient modes are the most relevant clinical scenarios (i.e. CP and “Best shim” for mother and foetus) and they are highlighted in figure 1 (blue box region). The graphs show that for the simulation targeting a constant B1+, the constrained SAR values for all shimming cases, including worst case SAR (cases 1-5 in figure 1), are lower than the CP values reported to be acceptable in Ref. 2. This finding is also in agreement with the general conclusions in reference [4]. In summary, RF shimmed scanning of pregnant women in 3T MRI systems restricted to normal operating mode, can result in acceptable SAR levels when the whole system behaviour and the total system constrains (e.g. B1+rms, SAR model, target shimming function, power limitations) are taken into account.
Acknowledgements
No acknowledgement found.References
[1] IEC, “Medical electrical equipment - Part 2-33, Edition 3.2, IEC 60601-2-33:2010+AMD1:2013+AMD
[2] Murbach M., et al., Mag. Res. Med. 76 (2016), p.986.
[3] Boulant N., et al, ISMRM MR Safety workshop (2019).
[4] Harvey P., Zhai Z., Morich M., et al., Proc. of the 17th Meeting of ISMRM (2009), p4786.