4148
Noise navigator: An independent method to detect physiological motion during MRI-guided radiotherapy1Radiotherapy, UMC Utrecht, Utrecht, Netherlands, 2Computational Imaging Group for MRI Diagnostics & Therapy, Center for Image Sciences, UMC Utrecht, Utrecht, Netherlands, 3Research and Practical Clinical Center of Diagnostics and Telemedicine Technologies of the Moscow Department of Healthcare, Moscow, Russian Federation
Synopsis
The noise navigator provides physiological motion detection completely independent of the imaging volume or contrast of the MR images and can be acquired on a much faster (millisecond) time scale than MRI. We believe that the noise navigator can be used as an independent verification method to detect the occurrence of motion in synergy with real-time MRI-guided radiotherapy and standalone during e.g. recontouring when typically no MRI is performed. For abdominothoracic radiotherapy, we investigated bulk motion and variable breathing as these have a relatively large amplitude (millimeters). Additionally, swallowing detection was investigated given its complications for head-and-neck radiotherapy.
Introduction
Physiological motion during radiotherapy treatments could lead to potential underdosage of the tumor, and/or overdosage in organs-at-risk. With a hybrid MRI-linac system, the MR images acquired during treatment can provide the necessary motion information. A drawback of MRI-based motion monitoring is that 3D MR acquisitions, which are required to monitor all anatomy, are relatively slow (seconds). Additionally, while monitoring the motion with MRI, it is impossible to simultaneously acquire clinical MR images.To circumvent these drawbacks, we propose an additional alternative motion detection method, i.e. the noise navigator. The noise navigator originates from the ever-present thermal noise measured by the RF receive coils used for MR acquisitions1 and thus could provide motion detection completely independent from MRI by silent passive noise measurements during periods MRI is not typically acquired (e.g. recontouring). Additionally, the noise navigator is affected by all anatomic changes within the body volume close to the RF coil2 and is thus provides an alternative way to detect the occurrence of various types of physiological motion. Finally, the noise navigator does not depend on the imaging volume or contrast of the MR images and can be acquired on a much faster (millisecond) time scale than MRI. We believe that the noise navigator can be used as an independent verification method to detect the occurrence of motion in synergy with real-time MRI-guided radiotherapy and standalone during e.g. recontouring when typically no MRI is performed.
For abdominothoracic radiotherapy, we investigated bulk motion and variable breathing as these have a relatively large amplitude (millimeters). Additionally, swallowing detection was investigated given its complications for head-and-neck radiotherapy3.
Methods
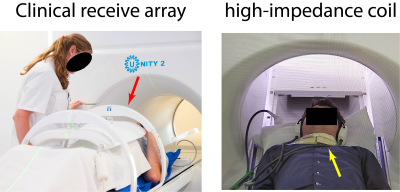
Ten healthy volunteers (five male and five female) were scanned on a 1.5T MRI-linac system (Unity, Elekta AB, Sweden).For bulk motion and breathing detection, signal was acquired with a clinically used receive array consisting of a 4 channel posterior array located in the table and 4 channel anterior array placed on a coil bridge (see Figure 1). A 2D balanced gradient echo cine MRI (50° flip angle, TR/TE=3.4/1.69 ms, 2x2x7 mm voxels, 560x280 mm FOV, 0.625 halfscan, SENSE 1.6, and 1 MHz receive bandwidth) was continuously acquired for 350 repetitions (186 ms temporal resolution). The 2D cine MRI slice was placed transversely for bulk motion detection, whereas a sagittal slice through the liver and right kidney was used for variable breathing detection. Each volunteer performed two experiments in which sudden bulk motion was simulated, and four experiments with variable breathing patterns.
For swallowing detection, experiments were performed with a radiolucent high-impedance coil4 on the neck (see Figure 1). High-impedance coils are compatible with MRI-guided radiotherapy and are especially suitable for head-and-neck5. A transversal 2D spoiled gradient echo cine MRI (4° flip angle, TR/TE=4.6/2.2 ms, 2x2x10 mm voxels, 560x150 mm FOV, 0.625 halfscan and 1 MHz receive bandwidth) through the larynx was continuously acquired for 200 repetitions (216 ms temporal resolution) during which the volunteer swallowed between two and four times.
The deformation vector fields were calculated from the 2D cine MR images with an optical flow (OF) algorithm6,7 to serve as a reference for displacement in all three experiment types. For validation, the mean absolute correlation between the noise navigator and OF-displacement was calculated.
Results
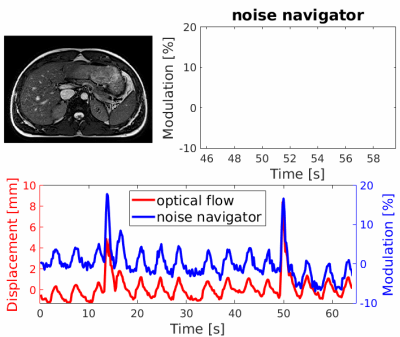
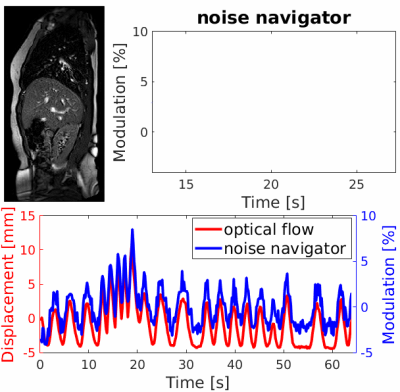
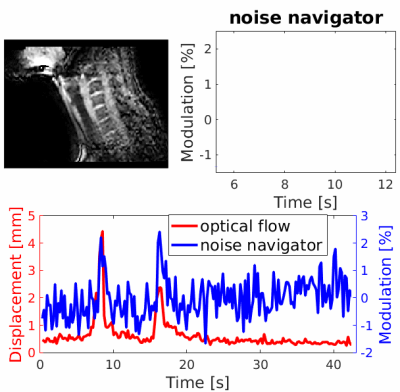
Figure 2 shows the OF-displacement and noise navigator during an experiment containing two bulk motion events (at 14 and 50 seconds). The observed periodic modulation was caused by respiration. Figure 3 shows the OF-displacement and noise navigator for an experiment where the breathing frequency varied over time. Figure 4 shows the displacement and noise navigator during an experiment containing two swallowing events (at 9 and 17 seconds).The mean absolute correlation between the OF-displacement and noise navigator over all measurements was 0.81, 0.9 and 0.32 for bulk motion, variable breathing and swallowing, respectively.
Discussion & Conclusion
A good correlation was observed between the OF-displacement and noise navigator for a total of sixty experiments (including bulk motion and variable breathing) in ten healthy volunteers. This good correlation between the noise navigator and displacement potentially means that the noise navigator with a simple linear model could yield fast (millisecond temporal resolution) 1D quantitative displacement.For the twenty swallowing experiments in ten volunteers, the observed correlation was poor. As seen in Figure 3, swallowing events were clearly detectable, yet the temporal correlation was low due to the noisy baseline. In this feasibility study, only a single high-impedance coil was used. However, we believe that swallowing detection could be improved by utilizing all receive channels within a head-and-neck array5.
In addition to motion detection for radiotherapy guidance, the ability of the noise navigator to detect physiological motion on a read out basis offers the potential to reduce the impact of motion artifacts. For instance the detection of swallowing could be used to discard certain readouts that would corrupt image quality8.
The noise navigator as shown here was unfiltered, thus the method could be further improved by optimizing the post-processing of the measured signal.
Acknowledgements
No acknowledgement found.References
[1] R.J.M. Navest, A. Andreychenko, J.J.W. Lagendijk, and C.A.T. van den Berg, “Prospective Respiration Detection in Magnetic Resonance Imaging by a Non-Interfering Noise Navigator,” IEEE Transactions on Medical Imaging, vol. 37, pp. 1751–1760, aug 2018
[2] R.J.M. Navest, S. Mandija, A. Andreychenko, A.J.E. Raaijmakers, J.J.W. Lagendijk, and C.A.T. Berg, “Understanding the physical relations governing the noise navigator,” Magnetic Resonance in Medicine, vol. 82, pp. 2236–2247, dec 2019
[3] T. Bruijnen, B. Stemkens, C.H. Terhaard, J.J. Lagendijk, C.P. Raaijmakers, and R.H. Tijssen, “Intrafraction motion quantification and planning target volume margin determination of head-and-neck tumors using cine magnetic resonance imaging,” Radiotherapy and Oncology, vol. 130, pp. 82–88, jan 2019
[4] S.E. Zijlema, R.H.N. Tijssen, V.N. Malkov, L. van Dijk, S.L. Hackett, J.G.M. Kok, J.J.W. Lagendijk, and C.A.T. van den Berg, “Design and feasibility of a flexible, on-body, high impedance coil receive array for a 1.5 T MR-linac,” Physics in Medicine & Biology, vol. 64, p. 185004, sep 2019
[5] S.E. Zijlema, L. van Dijk, L.E.L. Westlund Gotby, M.G.M. Italiaander, R.H.N. Tijssen, J.J.W. Lagendijk, C.A.T. van den Berg (2019) A mask-compatible, radiolucent head and neck receive array for MRI-guided radiotherapy treatments and pre-treatment simulation. Procs. MRinRT 2019
[6] C. Zachiu, N. Papadakis, M. Ries, C. Moonen, and B. Denis de Senneville, “An improved optical flow tracking technique for real-time MR-guided beam therapies in moving organs,” Physics in Medicine and Biology, vol. 60, no. 23, pp. 9003–9029, 2015
[7] C. Zachiu, B. Denis de Senneville, C. Moonen, and M. Ries, “A framework for the correction of slow physiological drifts during MR-guided HIFU therapies: Proof of concept,” Medical Physics, vol. 42, no. 7, pp. 4137–4148, 2015
[8] R.J.M. Navest, T. Bruijnen, J.J.W. Lagendijk, A. Andreychenko, and C.A.T. van den Berg, “Noise navigator based motion detection and compensation,” in Proc. Intl. Soc. Mag. Reson. Med. 26, (Paris), p. 702, 2018
Figures