4141
A Noval MR-Compatible and Clinically Available Microwave Needle for Spherical Ablation: Design and Ex Vivo Validation at a 0.7T1University of Science and Technology of China, Hefei, China
Synopsis
A novel MR-compatible microwave needle is proposed to achieve spherical ablation and monitor the temperature of needle shaft. It has an asymmetrical dipole choke with titanium alloy tube and a conical tip made of solid zirconia to facilitate needle insertion into tissues. FDTD simulations are used to minimize reflection coefficient and maximize aspect ratio. This most optimal design was validated in ex vivo pork liver in a 0.7T open MR system and concluded an acceptable artifacts, reflection coefficient of -27.86 dB and near-spherical ablation zone with a length of 39.5 mm, a diameter of 34.5 mm at 50W, 5 min.
INTRODUCTION
The majority of tumors are close to sphere, while conventional microwave antennas usually generate tear-shaped ablation zones and are ferro-magnetic or only for experimental use.1-3 This study aims to investigate a novel MR-compatible microwave needle for ablation therapy under MR guidance that not only satisfies the clinically available mechanical properties but also treats tumor with spherical ablation zone and monitors the temperature of needle shaft which is cooled by water circulation to avoid burning normal tissues.MATERIALS AND METHODS
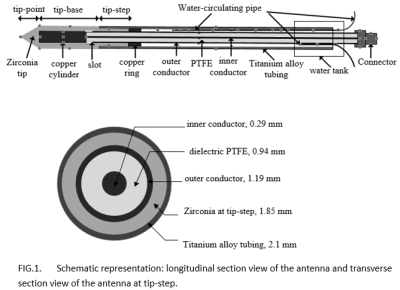
The minimally invasive MR-compatible microwave needle was designed to be an asymmetrical dipole choke antenna with titanium alloy tube and a conical tip made of solid zirconia to facilitate needle insertion into tissues. The temperature of needle shaft was controlled by water cooling circulation and monitored in real time by MR-compatible thermocouple which was specially processed. The most optimal design was obtained by FDTD simulations to minimize the reflection coefficient and maximize the diameter-to-length aspect ratio of ablation zone. Then the most optimal needle was fabricated to evaluate metal artifacts in a phantom study at 0.7T using FSE sequences with insertion orientation to the main magnetic field varying from 0°to 90°. Needle artifacts were measured by drawing a line perpendicular to the shaft into the image.4 S-parameters were measured by a network analyzer and compared with numerical results. Ex vivo experiments were performed using fresh pork livers for 2-10 min with input power of 30, 50 W respectively at 0.7 T. The ablation diameter, length and aspect ratio were measured and compared. Aspect ratios closer to 1 reflected a more spherical ablation zone.5RESULTS
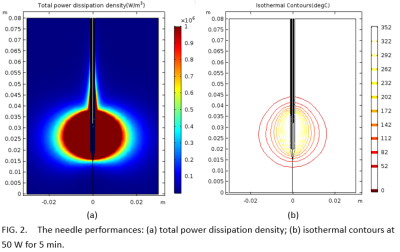
The needle performance was highly sensitive to antenna geometry. The most optimal design utilized the tip-base length of 15.6 mm, the tip-step length of 5.0 mm, the copper cylinder length of 12.0 mm and the slot length of 2.0 mm. It had a localized specific absorption rate focused on the needle tip and reflection coefficient of -33.91 dB at 2.45 GHz. The needle performance also changed with the relative permitivity of surrounding tissue during ablation process. Artifact widths of needle ranged from 2.35 mm to 5.66 mm when insertion angles ranged from 0° to 90° versus magnetic field using FSE sequence. In ex vivo studies, the most optimal needle with reflection coefficient of -27.8 dB created ablation zones with aspect ratio ranged from 0.75 ±0.03 to 0.92 ± 0.02 at 30, 50 W for 2, 5 and 10 min, respectively. The ablation diameters and lengths ranged from 20.2 ± 0.5 mm, 27.1 ± 0.9 mm at 30 W for 2 min to 37.9 ± 0.7 mm, 41.4 ± 1.3 mm at 50 W for 10 min, respectively. The ablation zone was nearly spherical.DISCUSSION
The MR-compatible microwave needle had an acceptable artifacts in the 0.7 T open MR system and created a nearly spherical ablation zone with low reflection coefficient.CONCLUSION
The minimally invasive MR-compatible microwave needle for nearly spherical ablation may be clinically available to treat tumors effectively in MR-guided interventions.Acknowledgements
The author wishes to thank Zhou Yufu for his support and discussions related to this work, thank Liu Zhengrong for his assistance with experimental data collection.References
1. Cavagnaro M, Amabile C, Bernardi P, et al. A minimally invasive antenna for microwave ablation therapies: design, performances, and experimental assessment[J]. IEEE Transactions on Biomedical Engineering, 2010, 58(4): 949-959.
2. Morikawa S, Inubushi T, Kurumi Y, et al. MR‐guided microwave thermocoagulation therapy of liver tumors: Initial clinical experiences using a 0.5 T open MR system[J]. Journal of Magnetic Resonance Imaging: An Official Journal of the International Society for Magnetic Resonance in Medicine, 2002, 16(5): 576-583.
3. Kaltenbach B, Roman A, Eichler K, et al. Real-time qualitative MR monitoring of microwave ablation in ex vivo livers[J]. International Journal of Hyperthermia, 2016, 32(7): 757-764.
4. Thomas C, Wojtczyk H, Rempp H, et al. Carbon fibre and nitinol needles for MRI-guided interventions: first in vitro and in vivo application[J]. European journal of radiology, 2011, 79(3): 353-358.
5. Hoffmann R, Rempp H, Erhard L, et al. Comparison of four microwave ablation devices: an experimental study in ex vivo bovine liver[J]. Radiology, 2013, 268(1): 89-97.
Figures