3918
Aberrant Regional Homogeneity in Bipolar disorder and schizophrenia: a meta-analysis of resting-state functional MRI1Medical Imaging Center, First Affiliated Hospital of Jinan University, Guangzhou, China, 2Department of Radiology, Six Affiliated Hospital of Sun Yat-sen University, Guangzhou, China, 3MR Research, GE Healthcare, Beijing, China
Synopsis
Resting-state functional MRI (RS-fMRI) studies have provided evidences for abnormal intrinsic brain activity in both schizophrenia and Bipolar disorder, but results are inconsistent. We conducted a meta-analysis of whole-brain, RS-fMRI studies to explore the Regional Homogeneity (ReHo) differences between patients with bipolar disorder (BD) and schizophrenia(SCZ). Our results suggested that the brain regions with convergent changes of ReHo in SCZ and BD included the Insular and prefrontalis lobe. While, the occipital lobe showed divergent change, where the ReHo value in SCZ decreases more. Patients with SCZ demonstrated much more widespread brain functional damage, including the decreased ReHo in sensorimotor area.
Introduction
Bipolar disorder (BD) and schizophrenia(SCZ) are severe and highly complex mental disorders with remarkable heterogeneous symptoms characterized by combinations of dysfunctions in thoughts, perceptions, emotions and behavior.1 Although BD and SCZ are clinically distinct disorders, convergent evidence suggests that there are no clear distinguishing borders between diagnostic categories for patients with mental disorders.2 Resting-state functional MRI(rs-fMRI)has proven useful for investigating the pathophysiological mechanisms of mental illness.3 Although the majority of analytic techniques [functional connectivity (FC), graph theory, independent component analysis (ICA), etc.for rs-fMRI data characterize the function of brain network, the local activity cannot be fully addressed with these approaches. Regional Homogeneity (ReHo) is the most widely used to provide information about local activity within a small region of the brain and is strongly recommended as an algorithm for BD and SCZ studies.4,5 Some of the inconsistent findings of studies comparing ReHo in BD and SCZ might be related to low statistical power of individual studies as most of the available studies have small sample sizes. A meta-analysis can be helpful to increase statistical power and provide an estimate of the level of differences in ReHo between BD and SCZ. The aim of the present review is using meta-analytic methods to evaluate published studies which compared the changes of ReHo value in each brain region in patients with BD or SCZ. We hypothesized that the change of brain imaging would be associated with the clinical symptom of BD and SCZ.Methods
First, we conducted a comprehensive search of studies published between January 1, 2000, and October 1, 2019, using the PubMed, Cochrane, Web of Science, SinoMed, Chinese National Knowledge Infrastructure and WanFang databases of a total of 36 articles. A meta-analysis of ReHo differences between patients and HCs was conducted for SZ and BD separately using the Seed-based d Mapping (SDM) software package (version 6.11 for Windows) in a standard process (www.sdmproject.com). We performed the analysis as described in the SDM tutorial and related publications and used MRIcron software (www.mricro.com/mricron/) to visualize SDM maps. Then a heterogeneity analysis was conducted using a random effects model with Q statistics to explore unexplained between-study variability in the results. At last Meta-regression analyses were carried out to examine the effects of clinical variables (e.g., illness duration, Positive Syndrome Score (PS), Negative Syndrome Score (NS) and General Syndrome Score (GS) for SZ; illness duration, Hamilton depression rating scale [HAMD] score and Young mania rating scale score [YMRS] for BD), which could potentially influence the analytic results.Results and disscusion
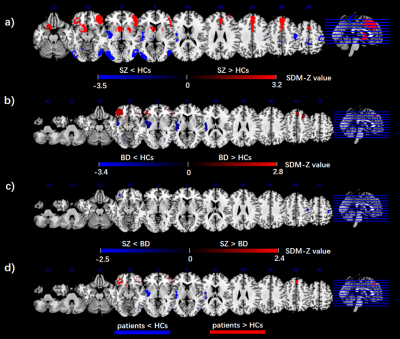
1. As illustrated in Fig. 1a, the meta-analytic brain map showed both increased and decreased ReHo in SZ patients relative to HCs. Patients with SZ displayed increased ReHo in the bilateral superior frontal gyrus, bilateral middle frontal gyrus, bilateral inferior frontal gyrus, bilateral anterior and median cingulate gyrus, right insula, and left striatum, and decreased ReHo in the bilateral middle temporal gyrus, bilateral inferior temporal gyrus, bilateral paracentral gyrus, bilateral postcentral gyrus, left insula, left superior temporal gyrus, left middle occipital gyrus compared with HCs.2. As illustrated in Fig. 1b, the meta-analytic brain map showed both increased and decreased ReHo in BD patients relative to HCs. Patients with BD displayed increased ReHo in the bilateral superior frontal gyrus, bilateral middle frontal gyrus, bilateral inferior frontal gyrus, and left striatum, and decreased ReHo in the left superior temporal gyrus, left middle temporal gyrus, left insula, left postcentral gyrus and left lingual gyrus compared with HCs.
3. As illustrated in Fig. 1c, the meta-analytic brain map showed decreased ReHo in SZ patients relative to BD patients.
4. As illustrated in Fig. 1d, the conjunction analysis revealed that both SZ and BD had increased ReHo in the bilateral superior medial frontal cortex and bilateral inferior orbital frontal cortex, and decreased ReHo in the left insula extending to superior temporal cortex compared with HCs.
5. In patients with SZ, meta-regression analysis indicated that longer illness duration was correlated with greater increase in ReHo of the right insula, and higher PS score was correlated with greater decrease in ReHo of the right middle occipital gyrus. In patients with BD, meta-regression analysis indicated that longer illness duration was correlated with greater decrease in ReHo of the left cuneus cortex, and higher HAMD score was correlated with greater decrease in ReHo of the left insula.
Conclusion
Our comprehensive meta-analysis suggests that the changes of ReHo in some brain regions of SCZ and BD are consistent involved the Insular lobe and prefrontalis lobe. There are also areas that change inconsistently in the occipital lobe of SCZ where the ReHo value decreases more. Patients with SCZ demonstrated much more widespread brain functional damage, including the decrease of ReHo in sensorimotor area, contributing to our understanding of the progressive pathophysiology of SCZ and BD.Acknowledgements
No acknowledgement found.References
1. Vigo, D., Thornicroft, G., and Atun, R. (2016). Estimating the true global burden of mental illness. The lancet. Psychiatry 3, 171-178.
2. Baker, J.T., and Dillon, D.G. (2019). Functional connectomics of affective and psychotic pathology. 116, 9050-9059.
3. Takamura, T., and Hanakawa, T. (2017). Clinical utility of resting-state functional connectivity magnetic resonance imaging for mood and cognitive disorders. Journal of neural transmission (Vienna, Austria : 1996) 124, 821-839.
4. Zang, Y., Jiang, T., Lu, Y., He, Y., and Tian, L. (2004). Regional homogeneity approach to fMRI data analysis. NeuroImage 22, 394-400.
5. Vargas, C., Lopez-Jaramillo, C., and Vieta, E. (2013). A systematic literature review of resting state network--functional MRI in bipolar disorder. Journal of affective disorders 150, 727-735.