3357
Prospective motion correction using real-time FID navigator motion measurements1Computational Radiology Laboratory, Boston Children's Hospital, Boston, MA, United States, 2Harvard Medical School, Boston, MA, United States, 3Advanced Clinical Imaging Technology, Siemens Healthcare, Lausanne, Switzerland, 4Radiology, Lausanne University Hospital and University of Lausanne, Lausanne, Switzerland, 5LTS5, École Polytechnique Fédérale de Lausanne (EPFL), Lausanne, Switzerland
Synopsis
FIDnavs can be acquired extremely rapidly using standard scanner hardware and are consequently an attractive tracking strategy for prospective motion correction (PMC), which requires accurate pose updates to be passed to the sequence with minimal delay. In this work, we demonstrate for the first time the efficacy of PMC using FIDnav motion estimates in a moving phantom and in volunteers performing deliberate head motion. Real-time pose updates from measured FIDnavs enabled substantial improvements in image quality in structural scans acquired with motion. FID-navigated PMC is a promising method for motion-robust imaging of patients who have difficulty staying still during imaging.
Introduction
Motion artifacts remain a major challenge for acquiring high-quality MRI in uncooperative subjects. Prospective motion correction (PMC) aims to compensate for motion-induced errors in spatial encoding by updating the imaging volume in response to measured changes in head position. However, successful PMC requires accurate pose estimates to be passed to the sequence with minimal delay to avoid introducing additional ‘pseudo-motion’ artifacts into the images.1 Free induction decay navigators (FIDnavs) have been shown to encode accurate rigid-body motion information2,3 and are highly suited for real-time applications as they can be rapidly acquired on the order of microseconds.4 In this work, we introduce a novel method for PMC using FIDnavs and an extended Kalman filtering (EKF) framework and demonstrate its ability to successfully compensate for motion in 3D structural imaging.Methods
Motion Model. Real-time motion tracking from FIDnavs was performed using the EKF algorithm with the following state-space model:5$$$\bf{x_k}=\bf{Ax_{k-1}}+\bf{w_k}$$$ with $$$\bf{w_k}\sim{N(0,\bf{Q_k})}$$$
$$$\bf{y_k}=\bf{Hx_k}+\bf{v_k}$$$ with $$$\bf{v_k}\sim{N(0,\bf{R_k})}$$$
where $$$\bf{x_k}$$$ contains the rigid-body motion estimates at time step $$$k$$$ and $$$\bf{y_k}$$$ is a vector of the real and imaginary components of the FIDnav. Head motion dynamics are modelled as a random walk, i.e. $$$\bf{A}=\bf{I}$$$. The measurement model $$$\bf{H}$$$ is a linearized approximation of how FIDnav measurements relate to underlying rigid-body motion parameters; $$$\bf{w_k}$$$ and $$$\bf{v_k}$$$ are Gaussian random vectors, with covariance $$$\bf{Q_k}$$$ and $$$\bf{R_k}$$$.
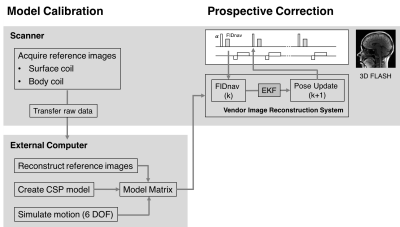
Model Calibration. To calibrate the system, low-resolution (4-mm)3 3D FLASH images, with contrast parameters designed to match the FIDnav, were acquired on the surface and body coils. Raw data was transferred to an external computer for image reconstruction and simulation of the effects of relative motion between the modeled coil profiles and the object. This calibration process (Fig. 1) was performed once at the beginning of each scan session.
FID-navigated PMC. An FIDnav module (20 samples in 125 μs; TNAV = 1 ms) was integrated into a 3D FLASH sequence every repetition time, following RF excitation and before the imaging readout. Complex FIDnav signals were averaged and used to update the EKF model parameters each TR. The Kalman gain, which controls the ratio between measurement and process noise, was chosen empirically ($$$K=0.001$$$) to give a reasonable trade-off between noise suppression and tracking ability. Motion estimates were calculated in the real-time processing unit of the vendor image reconstruction system and passed to the correction module in the sequence, which updates the applied gradients and RF pulses to compensate for rotational and translational motion (Fig. 1).
MRI Experiments. A pineapple was scanned at 3T (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) with a 64-channel head coil. Three consecutive FID-navigated 3D FLASH volumes (TE/TR=3.5/10 ms; FA=25°; RBW=400 Hz/px; matrix size=128x128x56; in-plane resolution 1.8 mm2; 4-mm slice thickness) were acquired with a single motion event during the second volume and PMC enabled. The accuracy of FIDnav motion estimates was assessed relative to rigid-body registration of image volumes acquired in both positions with PMC off.
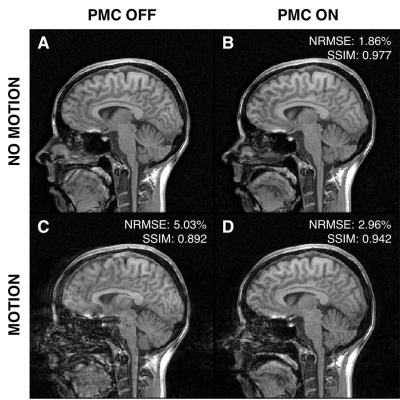
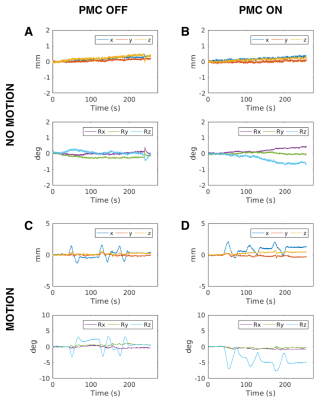
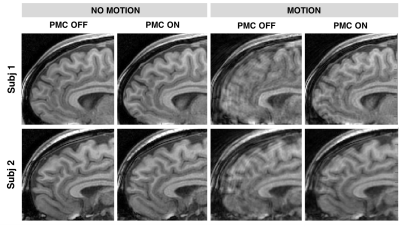
Two volunteers were scanned following written, informed consent. Four sagittal T1-weighted anatomical scans were acquired in each subject (TE/TR=4/10 ms; FA=30°; RBW=400 Hz/px; matrix size=256x256x128; in-plane resolution 1 mm2; 2-mm slice thickness) with and without deliberate motion (head shaking every 1-minute), and with and without PMC enabled. Normalized root-mean-square error (NRMSE) and structural similarity index (SSIM) were computed following rigid-body registration to the reference no-motion image.
Results
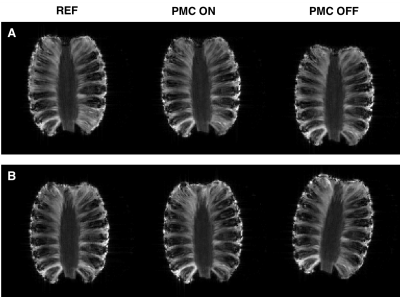
Sagittal views of the pineapple acquired with 18 mm translation along the z-axis (A) and 10° rotation around the x-axis (B), with and without PMC, are shown in Figure 2. FID-navigated PMC successfully maintained a fixed relationship between the object and scanner co-ordinate frame, with mean absolute errors of 1.1 mm and 1.2°.Figure 3 shows a four-way comparison between scans acquired with and without subject motion, and with and without PMC. The corresponding real-time motion estimates are shown in Figure 4, which are consistent with instructions given to subjects. In the no motion scans, FID-navigated PMC did not introduce any additional artifacts. In scans with deliberate head motion, a substantial reduction in ringing and blurring artifacts was achieved with FID-navigated PMC, compared to scans with PMC off (Fig. 5). Across both volunteers, NRMSE decreased from 4.33% ± 1.00% to 2.97% ± 0.01% with PMC; SSIM increased from 0.93 ± 0.05 to 0.97 ± 0.03.
Discussion
Our initial results demonstrate for the first time that online motion parameters can be estimated from ultra-short FIDnavs and prospectively applied to compensate for motion in 3D FLASH structural scans. Image quality was substantially improved in volunteers when PMC was enabled during motion. Residual artifacts may be due to small tracking errors or induced B0 field changes, currently not accounted for in the motion model. The total time required for reference data acquisition and processing was <5 minutes, which may be reduced in future iterations using on-scanner reconstruction and calibration. Unlike other navigator methods, which typically require sufficient dead time (~300-500 ms) to be present in the sequence, FIDnavs do not require spatial gradient encoding or image reconstruction, and the linearized model facilitates rapid, non-iterative motion estimation.Conclusion
FID-navigated PMC enables real-time motion compensation, without the need for specialized tracking hardware, which has potential to substantially improve structural MRI in uncooperative patient populations.Acknowledgements
This research was supported in part by NIH grants R01 EB019483, R01 NS079788, R01 DK100404, R44 MH086984, IDDRC U54 HD090255, and by an Early Career Award from the Thrasher Research Fund.References
1. Maclaren, J., Herbst, M., Speck, O. & Zaitsev, M. Prospective motion correction in brain imaging: A review. Magn. Reson. Med. 69, 621–636 (2013).
2. Babayeva, M. et al. Accuracy and precision of head motion information in multi-channel free induction decay navigators for magnetic resonance imaging. IEEE Trans. Med. Imaging 34, 1879–1889 (2015).
3. Wallace, T. E., Afacan, O., Waszak, M., Kober, T. & Warfield, S. K. Head motion measurement and correction using FID navigators. Magn. Reson. Med. 81, 258–274 (2019).
4. Kober, T., Marques, J. P., Gruetter, R. & Krueger, G. Head motion detection using FID navigators. Magn. Reson. Med. 66, 135–43 (2011).
5. Spincemaille, P., Nguyen, T. D., Prince, M. R. & Wang, Y. Kalman filtering for real-time navigator processing. Magn. Reson. Med. 60, 158–168 (2008).
Figures