3336
Feasibility of Tomoelastography in Inflammatory Bowel Disease: Preliminary Results1Radiology, Charité - Universitätsmedizin Berlin, Berlin, Germany, 2Surgery, Charité – Universitätsmedizin Berlin, Berlin, Germany, 3Medical Informatics, Charité - Universitätsmedizin Berlin, Berlin, Germany
Synopsis
Despite its success in the detection of inflammatory bowel disease (IBD), standard clinical MRI and other imaging modalities do not correlate with disease severity and cannot differentiate fibrotic and inflammatory bowel strictures. Anatomical details such as the descending colon and other parts of the intestine were demarcated on tomoelastography stiffness and fluidity maps, even without superimposed morphological images. Preliminary results demonstrate the feasibility of investigating IBD using tomoelastography. This study motivates larger trials and the assessment of fibrosis and inflammation in active IBD.
Introduction
Despite its success in the noninvasive detection of inflammatory bowel disease (IBD), standard clinical MRI and other imaging modalities do not correlate with disease severity and are limited in differentiating fibrotic and inflammatory bowel strictures.1 While fibrotic bowel strictures require endoscopic intervention or surgery, inflammatory bowel strictures benefit from anti-inflammatory treatment. This lack of an accurate diagnostic test restricts patient management. Tomoelastography by multifrequency MR elastography is a recently introduced advanced imaging method measuring viscoelastic tissue properties.2,3 Parameters are shear wave speed (SWS, in m/s) as a surrogate of stiffness, and shear modulus loss angle (φ in rad) which signifies the fluidity of the tissue (φ = 0 rad refers to pure solids, φ = π/2 rad refers to pure fluids). Tomoelastography compound maps are noise robust and display viscoelastic parameters with a pixel-wise resolution.2 Therefore, we aimed to investigate the feasibility of tomoelastography for the noninvasive assessment of patients with IBD.Methods
Seven patients with severe chronic IBD (ulcerative colitis, n = 5; Crohn's disease, n = 2; mean age of 45 ± 16 years, 3 female patients) underwent tomoelastography at 1.5 Tesla (Magnetom Aera, Siemens, Erlangen, Germany) using four externally placed custom-designed pressurized-air drivers and four mechanical drive frequencies of 40, 50, 60 and 70 Hz. Two abdominal drivers were placed anterior and posterior, respectively. Tomoelastography scan parameters were as follows: 25 axial slices, 8 offsets, 3 components, 300×198 mm2 field of view, 100×66 matrix size, 3×3×5 mm3 resolution, 55.8 Hz motion-encoding gradient (MEG) frequency, 31 mT/m MEG amplitude, TR 3070 ms, TE 50 ms, bandwidth 1000 Hz/Pixel, and Grappa factor 2. The total tomoelastography scan time was 5:17 min including acquisition of complete wave fields of all frequencies and two averages. Additionally, the scan protocol included a standard axial and coronal T2-weighted half-fourier acquisition single-shot turbo spin echo sequence. All patients were examined the day before scheduled surgical removal of the colon. Histopathological analysis of the surgical samples was used as the best diagnostic reference standard available. Three-dimensional region of interests (ROIs) were manually placed on axial elastograms focusing on IBD lesions of the lower third of the descending colon. Additionally, ROIs were placed on abdominal fat tissue for internal validation of the method. Statistical significance between IBD lesions and abdominal fat tissue was assessed using a two-sided t-test with a level of significance of P < 0.05.Results
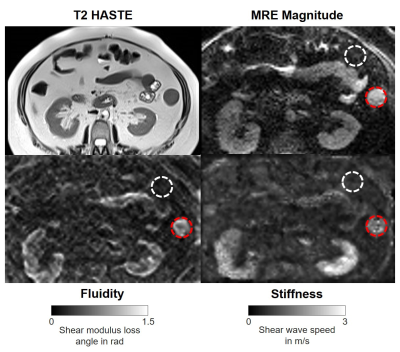
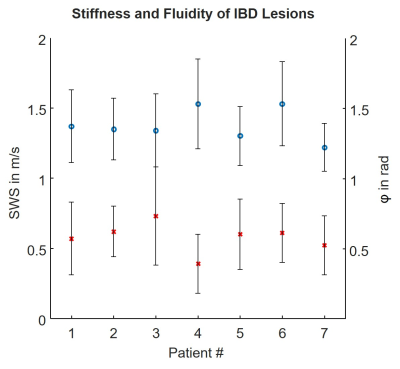
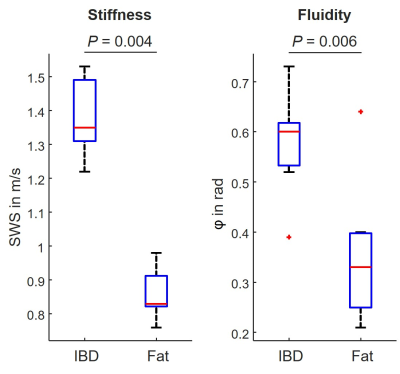
Tomoelastography was performed successfully on all included patients. A representative case of a patient with IBD is shown in figure 1. Axial ROIs including the IBD lesions were placed on average on 10 ± 7 slices with a median area of 13.28 cm3 (interquartile range of 40.30 cm3). Experimental data of SWS and φ for IBD lesions of all patients is shown in figure 2. Group mean values and standard deviations of SWS and φ were 1.38 ± 0.11 m/s and 0.58 ± 0.10 rad for IBD lesions, and 0.86 ± 0.07 m/s and 0.36 ± 0.13 rad for abdominal fat tissue (all P ≤ 0.006, respectively; figure 3).Discussion and Conclusion
Anatomical details such as the descending colon and other parts of the intestine were visually perceptible on both stiffness and fluidity maps without superimposed morphological images. IBD lesions showed significantly higher mean values of stiffness and fluidity than abdominal fat tissue. Supporting previous evidence of a case report, our results were in the same range as an acute appendicitis patient after antibiotic treatment with SWS of 1.47 ± 0.28 m/s and φ of 0.80 ± 0.11 rad.4 Preliminary results demonstrate the feasibility of investigating IBD using tomoelastography. This study motivates larger trials and the assessment of fibrosis and inflammation in active IBD.Acknowledgements
Funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation): RE 4161/1-1 (Rolf Reiter), RE 4161/1-2 (Rolf Reiter), RE 4161/2-1 (Rolf Reiter); Project Number 372486779 - SFB 1340 Matrix-in-Vision (Stephan Rodrigo Marticorena Garcia, Bernd Hamm, Jürgen Braun, Ingolf Sack and Patrick Asbach)References
1. Maaser C, Sturm A, Vavricka SR, et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019;13(2):144-164.
2. Tzschätzsch H, Guo J, Dittmann F, et al. Tomoelastography by multifrequency wave number recovery from time-harmonic propagating shear waves. Med Image Anal. 2016;30(5):1-10.
3. Muthupillai R, Lomas DJ, Rossman PJ, et al. Magnetic resonance elastography by direct visualization of propagating acoustic strain waves. Science. 1995;269(5232):1854-1857.
4. Marticorena Garcia SR, Hamm B, Sack I. Tomoelastography for non-invasive detection and treatment monitoring in acute appendicitis. BMJ Case Rep. 2019;12(8):e230791.
Figures