3320
Reducing TSM by Oxygen Inhalation: effective for pleural effusion but not ascites1Ridiology, The First Affiliated Hospital of Xi'an Jiao Tong University, xi'an, China, 2The First Affiliated Hospital of Xi'an Jiao Tong University, xi'an, China, 3MR Research China, GE Healthcare, xi'an, China
Synopsis
In this study, we try to provide a wider cohort of subjects with continuous low flow oxygen inhalation during dynamic contrast-enhancedMR liver imaging to reduce “Transient Severe Motion” (TSM) after administration of gadoxetate disodium.In addition, separate comparison of arterial phase motion scores was conducted among: category of combined Pleural Effusion, category of combined Ascites, and category of None.The results show that continuous oxygen can significantly reduce the occurrence of TSM; and 1) pleural effusion may reduce image quality, and can be alleviated by oxygen inhalation, and 2) oxygen inhalation is less effective under the condition of ascites.
Synopsis
In this study, we try to provide a wider cohort of subjects with continuous low flow oxygen inhalation during dynamic contrast-enhancedMR liver imaging to reduce “Transient Severe Motion” (TSM) after administration of gadoxetate disodium. The image quality was quantitatively assessed regarding to motion artifacts for each dynamic phases. The incidences of TSM were also compared between experimental and control groups. In addition, separate comparison of arterial phase motion scores was conducted among, according to the presence of complications, three divided categories: category of combined Pleural Effusion (including concurrent ascites), category of combined Ascites (including concurrent pleural effusion), and category of None.The results show that continuous oxygen inhalation can significantly reduce the occurrence of TSM; the observations can be summarized as: 1) pleural effusion may reduce image quality, and can be alleviated by oxygen inhalation, and 2) oxygen inhalation is less effective under the condition of ascites.Introduction
Radiologists have tried many ways to reduce the incidence of transient severe motion (TSM) associated with gadolinate disodium 1, despite existing reports only explain that gadolinate disodium can cause shortness of breath and decrease the holding time 2-4. The reported approaches include: four breath-holding commands were used circularly to keep the patient in inertia while injecting the contrast agent 5; reducing injection speed 6; dilute the gadolinate disodium but not reduce the injection rate 7, 8; inform and repeat breathing exercises 9; multi-arterial phase image acquisition method 10. Although these methods can reduce the incidence of TSM or reduce the impact on image quality, they do not solve the problem of breath-holding failure caused by drugs themselves. One recently published study from Namimoto et al 11 confirmed the role of oxygen inhalation in reducing motion artifacts, however, the sample size involved was relatively small, and subjects were limited to only those who had previously TSM. The purpose of our study is to evaluate the role of oxygen inhalation in reducing the incidence of TSM in gadolinate disodium enhanced liver imaging on a wider cohort of subjects.Methods
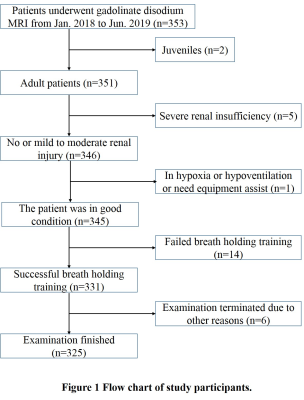
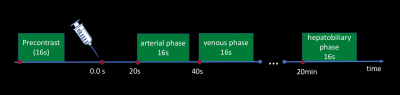
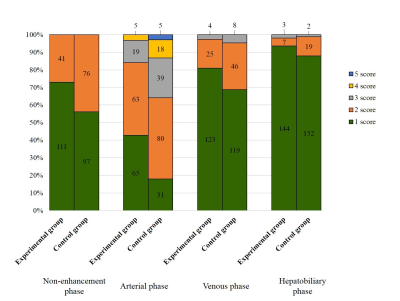
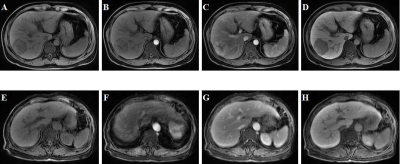
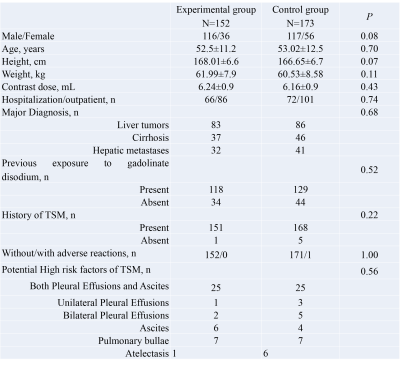
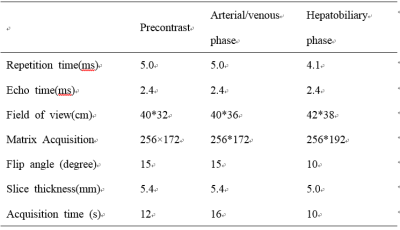
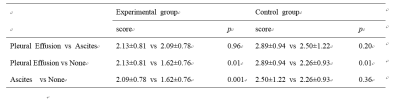
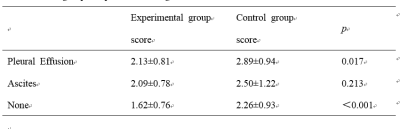
The Institutional Review Board approved this study and all the written informed consents were obtained from the patients or their family members.325 effective cases were included in this study (Fig 1). Demographic patient data was summarized in Table 1. Subjects were randomly divided into the experimentalgroup and the control group. Gadolinate disodium used in all patients was slowly and uniformly hand-administered intravenously at dose of 0.1 mL/kg by a qualified nurse. After the injection, 20 ml saline was flushed to ensure adequate dosage. During the examination, Patients in the experimental group weregiven oxygen of a low flow as 2L/min though nasal catheter, while those in the control group were not. All scans were performedon GE 3.0T MR scanner (Table 2) with 16 seconds scan time T1 FSPGR sequences (flow chart illustrated in Fig 2). After examination, each phase of dynamic T1-weighted images (precontrast, arterialphase, venous phase and hepatobiliary phase) was reviewed independently by two readers who were board-certified abdominalimaging fellows and were blinded to groups. Images were evaluated and scored for respiratory motion by using a scoring systemas follows: 1 = no motion artifact; 2 = minimal motion artifact, no impact on diagnosis; 3 = moderate motion artifact with some, butnot severe, impact on diagnosis; 4 = severe motion artifact, images degraded but interpretable; and 5 = extensive motion artifact,undiagnosable. TSM was considered present in examination when below 2 conditions are met 12: (a) arterial phase with an averagemotion score of at least 4 and (b) average motion scores of 2 or less on the precontrast phase, portal venous phase andhepatobiliary phase. In addition, separate comparison of arterial phase motion scores was conducted among, according to the presence of complications, three divided categories: category of combined Pleural Effusion (including concurrent ascites), category of combined Ascites (including concurrent pleural effusion), and category of None. The image quality and the incidence of TSM between the experimental group and the control group were putinto statistical analysis with SPSS version 20.0. t test, chi-square test, Kappa consistency test and Mann-Whitney U test were used. P value less than 0.05 was considered to indicate statistical significanceResults
The consistency of the subjective scores of arterial phase between the two radiologists was as Κ=0.892. Motion scores are summarized in Fig 3 and Fig 4. In the control group, the motion score was highest in arterialphase (2.34±0.99) and lowest in hepatobiliary phase (1.13±0.37), same as what was found in experimental group. Except that themotion scores in the experimental group were significantly lower (P<0.05). The incidence of TSM in the experimental group (3.29%,n=5) was significantly lower (P=0.01) than that in control group (13.29%, n=23). The intra-group and inter-group comparison results are summarized in Table 3 and Table 4 respectively.Discussion
The key finding of our study is low flow oxygen inhalation can effectively reduce the incidence of hepatic TSM enhanced by gadolinate disodium and can also improve the image quality of each phase from motion artifact, especially in the arterial phase. In addition,1) pleural effusion may reduce image quality, and can be alleviated by oxygen inhalation, and 2) oxygen inhalation is less effective under the condition of ascites.Acknowledgements
This study was supported by the National Natural Science Foundation of China (81971581, 81901823, 81771810), National Key Research and Development Program of China (2016YFC0100300), the 2011 New Century Excellent Talent Support Plan of the Ministry of Education of China (NCET-11-0438), the Project Funded by China Postdoctoral Science Foundation (2019M653659), and the Natural Science Basic Research Plan in Shaanxi Province of China (2019JQ-198).References
1. Davenport MS, Viglianti BL, Al-Hawary MM et al. Comparison of Acute Transient Dyspnea after Intravenous Administration of Gadoxetate Disodium and Gadobenate Dimeglumine: Effect on Arterial Phase Image Quality. Radiology, 2013;266:452–461
2. Akai H , Yasaka K , Nojima M , et al. Gadoxetate disodium-induced tachypnoea and the effect of dilution method: a proof-of-concept study in mice[J]. European Radiology, 2018;28:692-697
3 McClellan TR, Motosugi U, Middleton MS et al. Intravenous gadoxetate disodium administration reduces breathholding capacity in the hepatic arterial phase: a multi-center randomized placebo-controlled trial. Radiology, 2017;282:361–368
4 Hayashi T, Saitoh S, Tsuji Y et al. Influence of Gadoxetate Disodium on Oxygen Saturation and Heart Rate during Dynamic Contrast-enhanced MR Imaging. Radiology, 2015;276:756–765
5 Gutzeit A , Matoori S , Froehlich J M , et al. Reduction in respiratory motion artefacts on gadoxetate-enhanced MRI after training technicians to apply a simple and more patient-adapted breathing command[J]. European Radiology, 2016;26(8):2714-2722
6 Zech CJ, Vos B, Nordell A et al. Vascular enhancement in early dynamic liver MR imaging in an animal model: comparison of two injection regimen and two different doses Gd-EOB-DTPA (gadoxetic acid) with standard Gd-DTPA. Invest Radiol, 2009;44:305–310
7 Kim YK, Lin WC, Sung K et al. Reducing Artifacts during Arterial Phase of Gadoxetate Disodium-enhanced MR Imaging: Dilution Method versus Reduced Injection Rate. Radiology, 2017;283:429–437
8 Polanec SH, Bickel H, Baltzer PAT et al. Respiratory motion artifacts during arterial phase imaging with gadoxetic acid: Can the injection protocol minimize this drawback? J Magn Reson Imaging, 2017;46:1107–1114
9 Song J S , Choi E J , Park E H , et al. Comparison of transient severe motion in gadoxetate disodium and gadopentetate dimeglumine-enhanced MRI: effect of modified breath-holding method[J]. European Radiology, 2018;28(3):1132-1139
10 Grazioli L , Faletti R , Frittoli B , et al. Evaluation of incidence of acute transient dyspnea and related artifacts after administration of gadoxetate disodium: a prospective observational study[J]. La Radiologia Medica, 2018;123(12):910-917
11 Namimoto T , Shimizu K , Nakagawa M , et al. Reducing artifacts of gadoxetate disodium-enhanced MRI with oxygen inhalation in patients with prior episode of arterial phase motion: intra-individual comparison[J]. Clinical Imaging, 2018;52:11-15
12 Bashir MR, Castelli P, Davenport MS et al. Respiratory Motion Artifact Affecting Hepatic Arterial Phase MR Imaging with Gadoxetate Disodium Is More Common in Patients with a Prior Episode of Arterial Phase Motion Associated with Gadoxetate Disodium. Radiology, 2015; 274:141–148
Figures