3314
Noninvasive identification of renal perfusion in renal fibrosis of Adriamycin nephropathy by using ASL and IVIM-DWI imaging1Jiangsu Key Laboratory of Molecular Imaging and Functional Imaging,, Southeast University, Nanjing, Jiangsu, China, 2Clinical Science, Philips Healthcare, Shanghai, China
Synopsis
Renal fibrosis is the final common consequence of chronic kidney disease (CKD) and is the mechanism of CKD progressing to end-stage renal failure. Here we employed ASL and IVIM to assess longitudinal changes of kidney perfusion to reflect renal fibrosis in an animal model of ADR nephropathy. A significant decline in renal microcirculation was detected in the ADR group compared with the sham group. Administration of VCP979 could prevent the renal perfusion, and the treatment response was also detected by the two imaging technology.
Introduction
Renal fibrosis is the final consequence of chronic kidney disease (CKD) and is considered as the mechanism of CKD progressing to end-stage of renal failure[1]. Measurement of renal fibrosis is essential for treatment[2]. Here, we attempted to utilize arterial spin labeling imaging(ASL) and intravoxel incoherent motion diffusion weighted imaging(IVIM-DWI) to evaluate perfusion in animal model of renal fibrosis.Methods
24 male wistar rats were randomly divided into 3 groups: a) PBS-injection group(n = 8); b) ADR-injection vehicle group(n=8); c) ADR-injection + VCP1797 group(n=8). Treatments with ADR+VCP979 were initiated 4 weeks after ADR injection and maintained 4 weeks. The ASL based on FAIR and the IVIM-DWI with 10 b values (0-600s/mm2) of all groups were conducted on a 3T MRI scanner (Ingenia 3.0T, Philips Healthcare) at 4 and 8 weeks respectively after ADR injection. The ASL data were analyzed to obtain renal blood flow (RBF). The IVIM-DWI data were analyzed to obtain true diffusion coefficient (D), pseudo-diffusion coefficient (D*), and perfusion fraction(f). Finally, all rats were harvested and renal tissues were prepared for histological staining, including HE, Red Sirius and immunohistochemistry staining of CD31. The parameters of IVIM-DWI and RBF were performed to correlation with the parameters of histological staining.Results
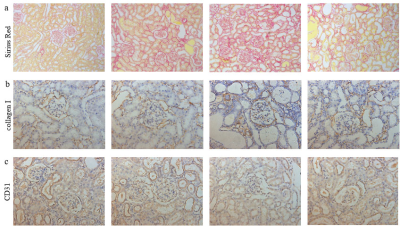
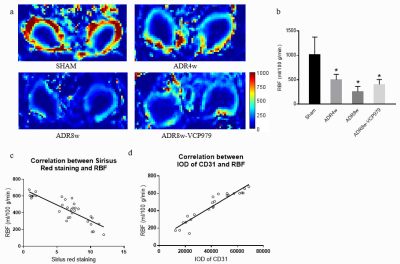
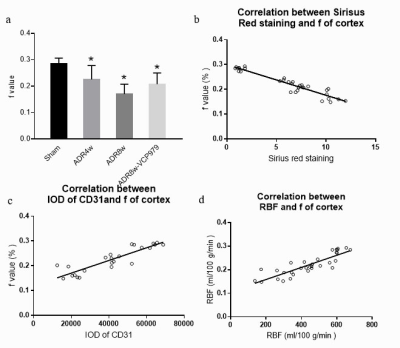
After ADR injection, renal perfusion significantly decreased after 4 weeks. Renal fibrosis was paralleled by progressive decline of perfusion after 8 weeks (Fig 1, Fig 2a&b). RBF showed a negative correlation with Red Sirius staining (r=-0.8624 , p<0.01), and a positive correlation with immunohistochemistry staining of CD31 (r=0.7082, p<0.01).Perfusion-related characteristic f obtained from IVIM decreased after the induction of renal fibrosis by 4 weeks ADR injection, and with a further reduction at 8 weeks(Fig 3a). The parameter of f showed significantly negative correlation with the area of fibrosis (r=-0.7974, p<0.01), and positive correlation with immunohistochemistry staining of CD31 (r=0.7296, p<0.01), Fig 3b&c. Furthermore, RBF showed a significant relationship with f (Fig 3d). However, D and D* did not show evident changes during the progression in ADR nephropathy.
Conclusion
In our study, the area of fibrosis was markedly increased in ADR nephropathy group compared with the sham group, and administration of VCP979 reduced the fibrotic area. Moreover, decreased microvascular was detected in the ADR nephropathy group, whereas VCP979-treatment group showed a recovery of microvascular. RBF and perfusion fraction(f) showed a prominent effect on evaluation of renal perfusion and were consistent with the results of histological staining. These two technology could detect the decline of renal microcirculation in renal fibrosis and evaluate the treatment response of VCP979.Acknowledgements
This work was supported by the National Nature Science Foundation of China (No.81830053, 81525014 ).References
1. Bai M, Chen H, Ding D, Song R, Lin J, Zhang Y, et al. MicroRNA-214 promotes chronic kidney disease by disrupting mitochondrial oxidative phosphorylation. Kidney Int. 2019;95(6):1389-404.
2. Gillis KA, McComb C, Patel RK, Stevens KK, Schneider MP, Radjenovic A, et al. Non-Contrast Renal Magnetic Resonance Imaging to Assess Perfusion and Corticomedullary Differentiation in Health and Chronic Kidney Disease. Nephron. 2016;133(3):183-92.
Figures