3075
Early experience in identifying chronic pelvic pain generators by sigma-1 receptor PET/MRI1Radiology, Stanford university, Stanford, CA, United States, 2Diagnostic, Molecular and Interventional Radiology, The Mount Sinai Hospital, New York, NY, United States, 3Gynecology, Stanford university, Palo Alto, CA, United States
Synopsis
Chronic pelvic pain is a highly prevalent pain condition among women, but it is quite challenging to determine the exact cause of pain. MRI is currently the imaging modality of choice, but even the most common etiology is very difficult to identify. In this abstract, we introduce a novel PET/MRI approach for chronic pelvic pain diagnosis to achieve improved sensitivity by enabling image tracking of sigma-1 receptor, a chaperone protein modulating ion channels for activating nociceptive processes. Our early results present promising results in identifying potential pain generators of chronic pelvic pain, which could not be detected in MRI alone.
Introduction
Chronic pelvic pain is a common medical condition affecting approximately 15% of women in westernized countries1, 2, but approximately half of patients with chronic pelvic pain lack a clear diagnosis2, 3. Additionally, half of patients have more than one potential cause of chronic pelvic pain4, which makes targeting the pain generator(s) challenging for treatment. The most common etiology of pelvic pain in women, endometriosis and adhesions, can be challenging to identify on MRI. Prior studies have shown that MRI has a high specificity but low sensitivity for detecting these pathologies, and up to 46% of patients with chronic pelvic pain that have no findings on MRI are found to have a gynecological structural cause on laparoscopy5.Sigma-1 receptors (S1R) are a unique class of intercellular chaperone proteins, which function in modulation of ion channels and other neurotransmitter systems associated with pain6. In vivo tracking of S1R became feasible with the recent development of 18F-FTC-146, a novel radiotracer highly specific to S1R7. This study investigates the use of this radiotracer for PET/MRI to localize the peripheral pain generator in women with chronic pelvic pain. We performed whole body 18F-FTC-146 PET/MR on chronic pelvic pain patients and compared the imaging results to those of asymptomatic controls.
Methods
This prospective observational study was approved by the institutional review board, and all subjects signed a written informed consent form. Five patients with chronic pelvic patients under the care of a gynecologist were recruited (ages 25-69). To qualify for the study, the patient had to have a minimum pain level of 4 on a 1-10 Comparative Pain Scale. Patients underwent a whole-body PET/MRI scan 30 minutes following the 10 mCi injection of 18F-FTC-146. 8-10 bed positions were adopted for the whole-body scan. In each bed position, 3D axial LAVA-FLEX, 2D axial T2w-FSE-FLEX sequences were performed. In the bed position covering the pelvis, multi-planar T1w and T2w 2D FSE sequences and the 3D axial DESS sequence were additionally performed.Images were reviewed independently by two radiologists to identify 18F-FTC-146 abnormalities in comparison to asymptomatic controls (n=5, ages 28-49). The diagnostic pelvic MR images were first reviewed to identify pathology that could contribute to the patient’s symptoms. The PET images were subsequently reviewed to look for significant abnormal uptake in comparison to the imaging pattern of normal controls. The co-registered PET/MRI images were then reviewed using the patient surveys regarding the location and laterality of pain at the time of imaging. The pelvic region was segmented in 5 tissue types (uterus, vagina, pelvic bowel, gluteus maximus, liver) and the standardized uptake value of 18F-FTC-146 was measured using Horos (version 3.3.2) with region-of-interest analysis. The abnormal image findings were later matched to the findings from the follow up treatments for validation.
Results
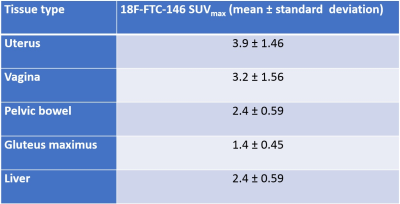
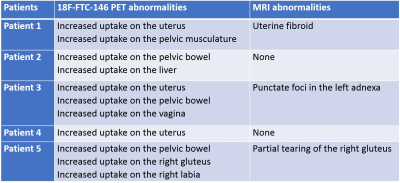
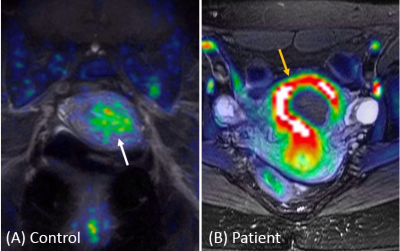
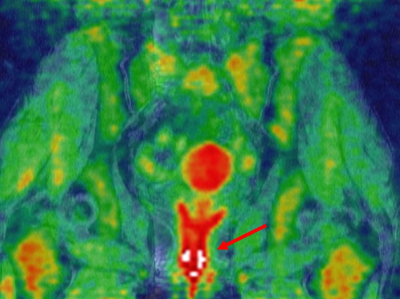
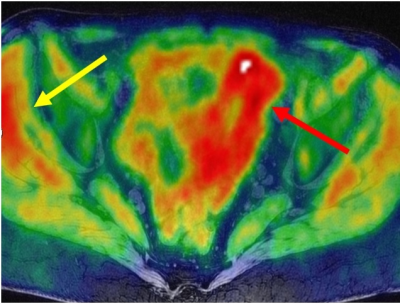
The 18-FTC-146 uptake in various segmented tissues within the asymptomatic controls is summarized in Figure 1. All five patients showed abnormally increased uptake of 18F-FTC-146 in comparison to controls with various diagnostic implications, whereas two patients did not present any abnormalities on MRI that could be related to the pain symptom (Figure 2). Figure 3 shows an example of abnormally increased uptake on uterus (SUVmax = 9.5) of a patient where the mean SUVmax of asymptomatic controls was 3.9. The patient underwent a laparoscopic hysterectomy with pathology showing an infarcted fibroid and endometriosis. Her pelvic pain ultimately resolved after hysterectomy. Figure 4 shows an example of the abnormally increased uptake on the vagina (SUVmax = 5.5). The mean SUVmax of controls was 3.2 (standard deviation = 1.56). The patient was found to have one lesion of endometriosis, which was excised and confirmed to be endometriosis on pathology. Her pain did improve postoperatively. Figure 5 presents a case of abnormally increased uptakes throughout the bowel (SUVmax = 13.6) and on the right gluteal muscle (SUVmax = 9.3). Note that the mean SUVmax of controls are 2.4 (bowel) and 1.4 (gluteal muscle).Discussion
In this work, we demonstrated the feasibility of 18-FTC-146 PET/MRI for identifying pain generators in patients with chronic pelvic pain. Given the many etiologies of chronic pelvic pain and that many patients have more than one cause of their pain, the complimentary approach of using both diagnostic MR and metabolic assessment with 18-FTC-146 provides a more comprehensive and inclusive evaluation.One of the most striking findings in our early results is the intense amount of uptake around the bowel in women who have previously had extensive lysis of adhesions and/or stage 4 endometriosis. Both entities are typically challenging to identify on imaging, and adhesive disease tends to be a diagnosis of exclusion.
Note that the size of patient and control groups in our study is limited. Therefore, incorporating a larger number of patients with known diagnoses would be necessary to further validate the image findings. Histologic analysis on the pathologic tissue samples acquired from surgery would be also desirable to establish the correlation between S1R upregulation and pain.
Conclusion
Our results demonstrate the potential use of 18F-FTC-146 PET/MR in identify sources of chronic pelvic pain that are currently challenging to diagnose with imaging, such as adhesive disease or distant endometrial implants.Acknowledgements
GE Healthcare, NIH P41 EB015891.References
1. Stein, SL. “Chronic Pelvic Pain.” Gastroenterol Clin N Am. 2013; 42: 785-800.
2. Ahangari A. “Prevalence of chronic pelvic pain among women: an updated review.” Pain Physician. 2014; 17(2): E141-E147.
3. Mathias SD, Kuppermann M, Liberman RF, et al. “Chronic pelvic pain: prevalence, health-related quality of life, and economic correlates.” Obstet Gynecol 1996;87(3):321-7.
4. Williams R, Hartmann K, Sandler R, et al. “Prevalence and characteristics of irritable bowel syndrome among women with chronic pelvic pain.” Ostet Gynecol. 2004;104(3):452-458.
5. Khan K, Tryposkiadis K, Tirlapur S, et al. “MRI versus laparoscopy to diagnose the main causes of chronic pelvic pain in women: a test-accuracy study and economic evaluation.” Health Technol Assess. 2018 Jul;22(40):1-92.
6. Su TP, Su TC, Nakamura Y, & Tsai SY. The Sigma-1 Receptor as a Pluripotent Modulator in Living Systems. Trends Pharmacol Sci. 2016;37(4):262-278.
7. Hjornevik T, Cipriano P, Shen B, et al. “Biodistribution and Radiation Dosimetry of 18F-FTC-146 in Humans.” J Nucl Med. 2017;58(12):2004-2009.
Figures