3011
Hyperpolarized 13C MRI Improves Sensivity of Pulmonary Inflammation Detection in an Acid Aspiration Rat Model of ARDS1Radiology, University of Pennsylvania, Philadelphia, PA, United States, 2Bioengineering, University of Pennsylvania, Philadelphia, PA, United States, 3Anesthesiology and Critical Care, University of Pennsylvania, Philadelphia, PA, United States, 4Surgery, University of Pennsylvania, Philadelphia, PA, United States, 5Physiology, University of Pennsylvania, Philadelphia, PA, United States
Synopsis
Elevated Hyperpolarized (HP) lactate-to-pyruvate ratio has previously been linked to pulmonary inflammation. In this study, we used a logistic regression model to assess the added value of HP lactate-to-pyruvate ratio as a predictive marker of lung inflammation. Our data suggests, the combination of metabolic and functional information improves both sensitivity of detecting lung inflammation than functional information alone.
Introduction
The systemic hypoxemia, pulmonary edema and atelectasis characteristic of acute lung injury and acute respiratory distress syndrome (ARDS) (1-3) are associated with histological findings of diffuse alveolar damage, which has a strong inflammatory component. Recent findings suggest that patients with the hyper-inflammatory sub-phenotype of ARDS have twice the mortality rate of other ARDS patients (1,4). Biomarkers that enable early detection and characterization of pulmonary inflammation may therefore be critical to improving patient outcomes by enabling earlier patient stratification and more sensitive monitoring of response to therapy (4,5). In our previous work we demonstrated a strong link between elevated HP lactate-to-pyruvate ratio and lung inflammation in a rat model of ARDS (6). In the study, we use a logistic regression model to assess the added value of HP lactate-to-pyruvate ratio as a biomarker to detect presence of pulmonary inflammation in a similar rat model. Our analysis shows that adding metabolic information to functional parameters measured during mechanical ventilation can potentially improve the sensitivity of detecting pulmonary inflammation.Materials and Methods
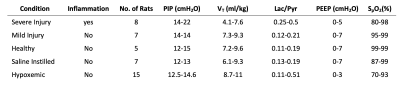
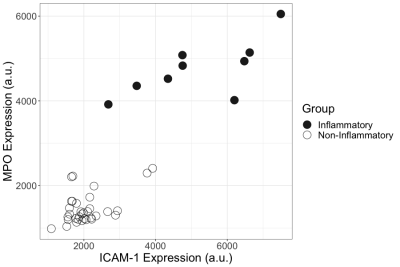
42 Sprague-Dawley rats were mechanically ventilated for four hours (VT=8 ml/kg, PEEP=5 cmH2O, FiO2=1, f=52 min-1). Animals were injured with instillation of 0.5ml/kg HCl as previously described (6). Hypoxia was induced by lowering the FiO2 to 0.10-0.17. Table 1 shows the summary of ventilation parameters are other measurement at the end of four hours. 13C HP-MRI was performed using a horizontal-bore 4.7T MRI system (Varian Inc.) as previously discussed (6). To assess the inflammatory status of the lung tissue, samples were collected and stained for markers of neutrophilic activity-myeloperoxidase (MPO)-and recruitment-intercellular adhesion molecule-1 (ICAM-1) at the end of each imaging session. K-means cluster analysis was performed on the ICAM-1 and MPO expressions to classify the lungs into inflammatory and non-inflammatory (Figure 2). A stepwise multivariate logistic regression model was developed for the prediction of inflammatory lungs. The model with the smaller Akaike information criterion (AIC) was selected. The same animals were used for both training and testing of the pre- diction model owing to the limited number of datasets, whereas a leave-one-out cross validation was performed for cross validation. One outlier data (cook’s distance > 0.1) was removed from the dataset. Workflow of the analysis is shown in Figure 3.Results and Discussion
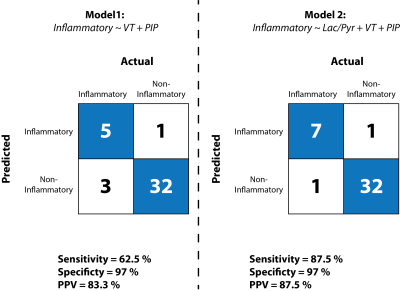
Our stepwise multivariate analysis shows that overall, lactate-to-pyruvate ratio along with peak inspiratory pressure (PIP) and tidal volume (VT) measured during ventilation have are the best predictors of inflammation among all independent variables. We compared the sensitivity, specificity and positive predictive value of this model in the presence and absence of lactate-to-pyruvate ratio as a predictor (Figure 4). We show that the lactate-to-pyruvate ratio improves the sensitivity and positive predictive value of our predictor but does not change the specificity of the model.Conclusions
In this study, we assessed the added value of hyperpolarized lactate-to-pyruvate ratio to detect presence of severe pulmonary inflammation in an acute model of lung injury in rats. Our data suggests that addition of metabolic information obtained from 13C HP-MRI to clinically relevant functional parameters measured during mechanical ventilation can potentially improve the sensitivity but not specificity of detecting pulmonary inflammation. A larger number of animals with various conditions may be required to further validate this finding. Nevertheless, this works shows the potential use of metabolic imaging markers to classify hyper-inflammatory phenotype in ARDS patients.Acknowledgements
This work was supported by NIH (Bethesda, MD, USA) grants R01-HL124986 and R01-HL139066.References
1. Thompson BT, of RCNEJ, 2017. Mass Medical Soc 2017;377:562–572. doi: 10.1056/NEJMra1608077.
2. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2012;307:2526–2533. doi: 10.1001/jama.2012.5669.
3. Johnson ER et al., Journal of Aerosol Medicine and Pulmonary Drug Delivery 2010;23:243–252. doi: 10.1089/jamp.2009.0775.
4. Calfee CS et al., The Lancet Respiratory Medicine 2018. doi: 10.1016/S2213-2600(18)30177-2.
5. Calfee CS et al., American journal of respiratory and critical care … 2016
6. Pourfathi M et al., nature.com 2018;8:280. doi: 10.1038/s41598-018-21901-0.
Figures