2812
Compression of nerve root causes high degree of fat infiltration of lumbar multifidus muscle1Department of Radiology, the First Affiliated Hospital, Xi'an Jiaotong University, xi'an, China, 2MR Research China, GE Healthcare, Bei Jing, China
Synopsis
The increase of multifidus muscle fat infiltration will affect the postoperative rehabilitation of patients with lumbar spine surgery. In this study, reasons for fat infiltration on both sides of multifidus muscles were analyzed retrospectively. Through Priffman grading evaluating the intervertebral disc and Kader grading for fat infiltration, a retrospective analysis was conducted on 453 cases of intervertebral discs images. In our study, nerve root compression was found to be correlated with degree of multifidus muscle fat infiltration. This correlation support the hyposis that nerve root compression would result in an increase in the adiposity of multifarious muscles.
Introduction
By measuring signal intensity of muscle on T2 weighted images, Maryse Fortin et al. concluded that there was greater fat infiltration on the side of the herniated disc1.A previous study performed histopathological analysis on multifidus muscle specimens has shown the nerve root compression by lumbosacral disc herniation causes paraspinalmuscle changes2. Hence, we presume that the compression of the nerve root could be the reason of muscle lipidization. This study retrospectively analyzed magnetic resonance (MR) lumber spine images. The level of nerve root compression and muscle lipidization were quantified by Priffman disc grading and the Kader grading system respectively. Therefore, the purpose of this study was to find the relationship between the degree of nerve root compression and the degree of multifidus muscle lipidization using conventional MRI images.Methods
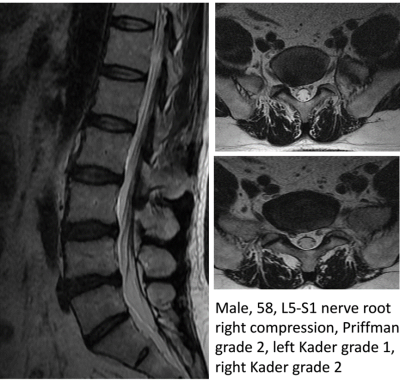
Images of all patients undergoing lumbar MRI in our center from January to April 2019 were retrospectively analyzed, and T2 SAG and T2 Ax images were selected.The level of intervertebral disc herniation was determined in sagittal position, and Priffman grading and Kader grading of intervertebral disc herniation in transverse position were conducted. Priffman grading 3 was performed Grade0 (normal): No compromise of the nerve root is seen. Grade 1 (contact): There is visible contact of disk material with the nerve root, and the normal epidural fat layer between the two is not evident. The nerve root has a normal position, and there is no dorsal deviation . Grade 2 (deviation): The nerve root is displaceddorsally by disk material . Grade 3 (compression): The nerve root is compressed between disk material and the wall of the spinal canal; it may appear flattened or be indistinguishable fromdisk material.Muscle atrophy of the Lumber multifidus(LMM) was graded in accordancewith the grading system described by Kader et al. 4.Briefly, Grade 0 was ascribed to an LMM of normal caliber with no fat streaks; Grade 1, defined as replacement of less than 10% of the LMM bulk; Grade 2 for moderate atrophy and fatty infiltration with lessthan 50% replacement of the muscle with fat and fibroustissue and Grade 3 for severe atrophy and fatty change with greater than 50% replacement of the muscle.(Fig 1)Basic information such as name, gender and age were collected.All statistical analysis were performed by using SPSS 20.0 (SPSS, Chicago, IL, USA); p<0.05 was considered as statistically significant difference.Results
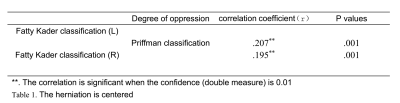
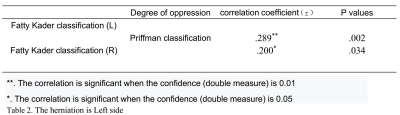
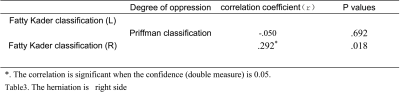
A total of 244 (110 male and 134 female) patients with the age(51±16)were enrolled in this study. Lumbar magnetic resonance imaging was performed in all patients , some patients had herniated discs at more than one vertebral level. So we analyzed a total of 453 problematic vertebral levels. According to the situation of disc herniation can be divided into central type and lateral recess type.Priffman grading and Kader grading were related to the central type. The degree of compression was correlated with the degree of aliphatization, and both sides were correlated, indicating that the higher the degree of compression was, the higher the degree of aliphatization was (the correlation coefficient r=0.207 on the left , r=0.195 on the right). (Table1)A herniated disc to the left had the same result (left correlation coefficient r=0.289,and the right r=0.200). (Table2)Disc herniation to the right can also indicate the correlation between degree of compression and degree of steatosis (left correlation coefficient r=-.050;right Correlation coefficient r=.292)(Table3).Discussion
Lumbar disc herniation is a common disease, usually accompanied by low back pain, limping lower limbs and other complications, posing huge impact on patients’ daily life. Grading according to the degree of prominence is also an important part of evaluating the degree of compression of nerve roots. A higher Priffman rating indicates a higher degree of nerve root compression, and a higher Kader rating indicates a higher degree of steatosis. The changes of multifiluid muscles have certain effects on patients' surgical outcome and postoperative rehabilitation5-6.The researchers noted that nerve root damage leads to atrophy of type 1 and type 2 fibers, and that the multifiluids only undergo structural changes at the site of involvement7. The proximity and severity of the disc degeneration had significant effects on the levels of IL-1βexpression in the multifidus muscle8. Gregory James et al macrophages and TNF (pro-infammatory cytokine) play an active role in the subacute/early chronic phase of remodeling in muscle, adipose and connective tissues of the multifdus during IVD degeneration9. In our study, the observed correlation between the Priffman score and the Kader score is in accordance with aforementioned studies. Preliminary results supports the hypothesis that nerve root compression would result in an increase in the adiposity of multifarious muscles. Future study with bigger cohort of subjects are warranted.Conclutions
The nerve root compression quantified by Priffman grading is correlated the degree of lipidization, also the inconsistently distributed degree of lipidization is higher in compression side. Those observations strongly support the hypothesis that nerve root compression is the reason of multifidus muscle fat infiltration.Acknowledgements
No acknowledgement found.References
1. Fortin M, Lazáry À, Varga P P, et al. Paraspinal muscle asymmetry and fat infiltration in patients with symptomatic disc herniation[J]. European Spine Journal, 2016, 25(5):1452-1459.
2. Franke J, Hesse T, Tournier C, Schuberth W, Mawrin C, LeHuec JC, et al. Morphological changes of the multifidus muscle in patients with symptomatic lumbar disc herniation. J Neurosurg Spine. 2009;11:710–4.
3. Pfirrmann C W A , Dora C , Schmid M R , et al. MR Image–based Grading of Lumbar Nerve Root Compromise due to Disk Herniation: Reliability Study with Surgical Correlation1[J]. Radiology, 2004, 230(2):583-588.
4. Kader DF, Wardlaw D, Smith FW. Correlation between the MRI changes in the lumbar multifidusmuscles and leg pain. Clin Radiol 2000; 55: 145-149.
5. Deyo R A, Mirza S K. CLINICAL PRACTICE. Herniated Lumbar Intervertebral Disk[J]. N Engl J Med, 2016, 374(18):1763-1772.
6. James G , Millecamps M , Stone L S , et al. Dysregulation of the Inflammatory Mediators in the Multifidus Muscle After Spontaneous Intervertebral Disc Degeneration SPARC-null Mice is Ameliorated by Physical Activity[J]. SPINE, 2018:1.
7. Yoshihara K , Shirai Y , Nakayama Y , et al. Histochemical Changes in the Multifidus Muscle in Patients With Lumbar Intervertebral Disc Herniation[J]. Spine, 2001, 26(6):622-626.
8. James G , Millecamps M , Stone L S , et al. Dysregulation of the Inflammatory Mediators in the Multifidus Muscle After Spontaneous Intervertebral Disc Degeneration SPARC-null Mice is Ameliorated by Physical Activity[J]. SPINE, 2018:1.
9. Gregory J , Sluka K A , Linda B , et al. Macrophage polarization contributes to local inflammation and structural change in the multifidus muscle after intervertebral disc injury[J]. European Spine Journal, 2018.