2810
Comparison of Meniscal T2* Metrics in Elite Basketball Players and Swimmers
Erin C Argentieri1, James C Yoder1, Garry Gold2, Sharmila Majumdar3, Matthew F Koff1, and Hollis G Potter1
1Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States, 2Stanford University, Stanford, CA, United States, 3University of California San Francisco, San Francisco, CA, United States
1Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States, 2Stanford University, Stanford, CA, United States, 3University of California San Francisco, San Francisco, CA, United States
Synopsis
As basketball players represent a population with an inherently high risk of sustaining meniscal injuries, studying how basketball play can lead to changes in the meniscus is of clinical importance. To date, no studies have been performed to evaluate T2* values of the meniscus in high performance athletes. Therefore, the purpose of this study was to utilize ultra-short TE (UTE) MRI to compare meniscal T2* values between basketball players and swimmers. Significant differences of T2* values were found between the medial and lateral menisci. No significant difference of meniscal T2* values were found between basketball players and swimmers.
Introduction
Basketball is played widely around the world, and while many consider it to be a non-contact sport, knee injuries are common in these athletes as the knee is repeatedly exposed to high loads during running, cutting and jumping activities.1 The menisci, located between the distal femoral and proximal tibial articular cartilages, work to absorb these loads and protect the underlying cartilage and bone during weight bearing activities. Acute damage to the meniscus often results from high compressive forces with concomitant flexion or rotation of the knee joint.2,3 Unfortunately these injuries are occurring with increasing frequency in young athletes and the presence of meniscal injuries or meniscal degeneration is highly correlated with subsequent degenerative joint disease.4 As basketball players represent a population with an inherently high risk of sustaining meniscal injuries, studying how basketball play can lead to changes in the meniscus is of clinical importance. Ultrashort echo (UTE) magnetic resonance imaging (MRI) can be used to effectively image the rapid transverse relaxation times associated with the menisci.5,6 In addition, the quantitative MRI (qMRI) metric of T2* has been shown to be correlated to meniscal degeneration.7 To date, no studies have been performed to evaluate T2* values of the meniscus in high performance athletes. Therefore, the purpose of this study was to compare meniscal T2* values between basketball players and swimmers.Methods
30 collegiate athletes (16 swimmers and 14 basketball players) were enrolled, with informed written consent, in a longitudinal multi-site study. MRI: Bilateral 3-Tesla MRI examinations were obtained on a clinical scanner (GE Healthcare, Waukesha, WI) using an 8-channel phased array knee coil (Invivo). Three-dimensional, CONES UTE sequences were acquired for evaluation of T2* metrics (Matrix: 256x256mm, Slice Thickness: 3.0mm, TEs: 5 echoes between 0.03-24ms, TR: 188ms, RBW: ±83.3kHz, Flip-Angle: 16o). All menisci were manually segmented using MeVisLab software, and T2* values were calculated (MatLab, Natick, MA) using a mono-exponential fit. Statistical Analysis: A two way repeated measures ANOVA was performed to evaluate the effects of sport (swimming/basketball) and knee compartment (medial/lateral meniscus) on T2*(SAS, V9.3, Cary, NC). Based on the ANOVA results, an unpaired t-test was performed to evaluate differences of meniscal T2* values between basketball players and swimmers for each compartment. Significance was set to p<0.05.Results
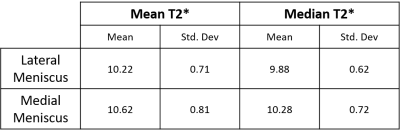
Significant differences in T2* metrics were found between the medial and lateral menisci for both median T2* and mean T2* values (p=<0.0005, Table 1). No significant differences were found between swimmers and basketball players for either compartment (p>0.05).Discussion
This study evaluated differences in medial and meniscal T2* values between the medial and lateral compartments and between sports. No differences between swimmers and basketball players were detected even though basketball players have reported higher compression and shear forces in their knee during play, as compared to swimmers. Differences detected between the medial and lateral menisci T2* metrics could be due to the biomechanics of the knee joint and the structure of the meniscus in response to how weight bearing is distributed between the medial and lateral compartments. For example, while both menisci are predominantly composed of highly ordered type 1 collagen fibers, the lateral meniscus has been found to have a thicker zone of uncalcified fibrocartilage and increased calcified tissue at the anterior and posterior horns compared to the medial meniscus8. Additionally, the medial and lateral menisci undergo disparate loading conditions: more than 50% of load in the lateral compartment is transmitted through the lateral meniscus, while the medial meniscus transmits approximately 50% of the medial compartment.9 The lack of differences of T2* between the basketball players and swimmers may be attributable to limited enrollment, and the need for further evaluation of meniscal subregions (anterior horn, meniscal body, posterior horn) to localize differences that may not be evident with a global analysis.Conclusion
This study found differences between medial and lateral meniscal T2* values, but differences were not found between sports. We anticipate that increase enrollment and regional analysis of the menisci will lead to regional differences between the sports. Future analysis will include comparison of meniscal T2* values with an assessment of the adjacent femoral and tibial articular surfaces. The current dataset was for the first visit of a longitudinal study. Differences in meniscal T2* values may be detected as subjects return for their follow-up visits at 12 and 30 months. Understanding the longitudinal changes of meniscal T2* values may help define the progression of meniscal degeneration in elite athletes.Acknowledgements
GE/NBA Research Consortium: The Advanced Imaging Protocol StudyReferences
- Zedde 2015, Joints
- Yeh 2012, AJSM
- Ripani 2012, J of Sports Traumatology
- Lohmander 2007 AJSM
- Gold 1995, MRM
- Gatehouse 2003, Clin Radiol
- Koff 2013, OAC
- Bloecker 2012, Cells Tissues Organs
- Stoller 2007, Lippincott Williams & Wilkins