2801
Subtle Intensity Graduating Homomorphic Transform with a Small-percentage of Fat-saturation to Improve Conspicuity of Meniscal Tears at 7T1Siemens Medical Solutions USA, Inc., Rochester, MN, United States, 2Department of Radiology, Mayo Clinic, Rochester, MN, United States
Synopsis
In this work, we propose the use of Subtle Intensity Graduating Homomorphic Transform (SIGHT) along with application of a small percentage of fat-saturation (fat-sat) to improve the conspicuity of meniscal tears at 7T. 2 musculoskeletal radiologists compared turbo-spin-echo (TSE) proton-density (PD)-weighted knee MRI (without fat-sat) with 12 different MRI options (TE, TR, fat-sat, field-of-view, and image-processing variations) for conspicuity of meniscal tears and rated 1st, 2nd and 3rd preferred options for each case. SIGHT image-processing applied to PD-weighted MRI along with a small percentage of fat-sat provided better conspicuity of meniscal tears than the regular PD- and T2-weighted MRI images.
Introduction
Detecting meniscal tears is an important component of routine knee MRI. Turbo-spin-echo (TSE)-based proton-density (PD)-weighted sagittal MR images without fat-saturation (fat-sat) are primarily used for detecting knee meniscal tears (1,2). The conspicuity of meniscal tears depends on multiple factors including: i) spatial resolution (or voxel size) of the MRI data; ii) dynamic range of the intensities in the image; iii) intensities of the regions around the menisci (in other words the contrast between meniscal region and the surrounding tissue); iv) receive intensity profile or coil sensitivity profile of the receive coil used; v) transmit B1 inhomogeneity at/near the menisci; vi) window width (WW) and window level (WL) used for visualizing the meniscal tears; and vii) Image post-processing. Some of these factors are applicable at all MRI field strengths, but factors such as receive and transmit inhomogeneity are accentuated at higher field strengths, especially at ultra-high field (UHF) such as 7T. Recently, a UHF 7T MRI system received FDA approval for clinical use, and addressing the challenges in meniscal tear conspicuity at 7T is of paramount importance for routine clinical use of 7T knee MRI. Recently, it was demonstrated that controlling the brightness of fat by applying a small percentage of fat-sat to PD-weighted TSE MRI (PD-MRI) improves the dynamic range of image intensities and consequently improves the conspicuity of meniscal tears at 3T and 7T (3). In this work, we propose the use of Subtle Intensity Graduating Homomorphic Transform (SIGHT) along with application of a small percentage of fat-sat to PD-MRI to further improve the conspicuity of meniscal tears at 7T.Methods
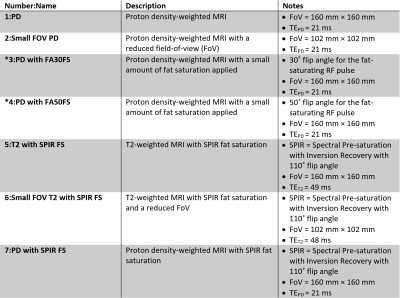
11 subjects with meniscal tears detected on a 3T MRI were recruited and imaged using a 28-channel receive, single-channel transmit knee coil (QED, Quality Electrodynamics, Mayfield Village, OH, USA) at 7T (MAGNETOM Terra, Siemens Healthcare, Erlangen, Germany) under the guidelines of an IRB.A prototype 2D TSE sequence was used to acquire the data described in Table 1 in a sagittal orientation.
SIGHT Method
If X is the voxel intensity, then the SIGHT transform (Y) is:
$$Y=\frac{X^{(p/q)}}{m^{(p/q)}}\times4095$$
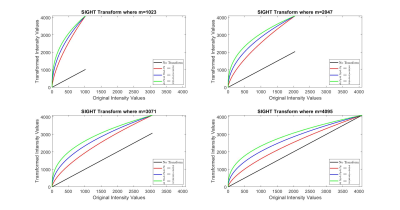
where m is the maximum intensity present in the MRI volume. The PD-MRI with FA30 FS and FA50 FS were processed with the SIGHT method using p/q values of 2/3 (SIGHT Option 1), 1/2 (SIGHT Option 2) and 2/5 (SIGHT Option 3) to improve the conspicuity of meniscal tears. Figure 1 shows the SIGHT transformation plots for different values of m and p/q.
Evaluation
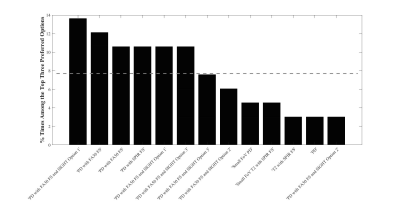
Two MSK fellowship trained radiologists evaluated the conspicuity of meniscal tears and selected the top 3 preferred options for each subject. The different sequence and image processing options were presented in a blinded and anonymized fashion for evaluation. The order in which the options were presented was also randomized for each subject. The full-FoV (160 mm × 160 mm) images were zoomed to the small FoV (102 mm × 102 mm) for comparison to blind the reviewers to the acquisition FoV. The intensity range used for display of all the PD-weighted options was the same (0-4095) for all comparisons. The intensity range used for display of the two T2-weighted fat-sat options (full FoV and small FoV) was the same (0-2047) for all comparisons.
Results and Discussion
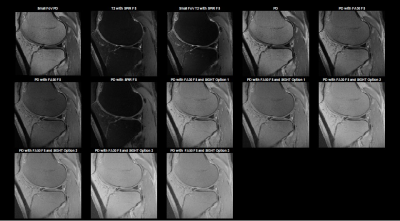
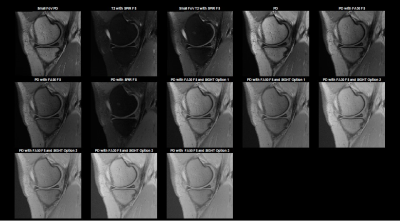
Figures 2 and 3 compare the meniscal tear conspicuity among the different options evaluated in this study at 7T for two representative subjects. Figure 4 shows the bar plot of the ratings provided by the radiologists.Fat affects the dynamic-range of the intensities and the contrast between the meniscal region and the bone marrow. If bone marrow is very bright, low intensity pathology such as meniscal tears near bone marrow would be less conspicuous with typical WW/WLs. DICOM typically uses 12 bits for intensity of an MR image, i.e. 0 to 4095 values in steps of 1. If there is a bright tissue (e.g. fat) in the FoV, regions with fat have intensity values close to 4095, while the meniscal regions (which typically have low intensity) will have values close to 0. By suppressing fat by a small percentage with a low flip angle (such as 30° or 50°) RF pulses, one can reduce the brightness of the fat and in turn improve the dynamic range of the image for visualization of low-intensity pathology such as meniscal tears.
The small-FoV options have a better dynamic range because the hyper-intensities proximal to the coil are not present in the small FoV.
Image transforms using SIGHT improved meniscal-tear conspicuity because the scaled power (p/q) transform with q value greater p as done with the SIGHT method optimized the dynamic range of intensities for better conspicuity of low-intensity pathologies such as meniscal tears.
Conclusions
SIGHT image processing applied to PD-weighted MRI with a small percentage of fat-sat improved the conspicuity of knee meniscal tears compared to PD- or T2-weighted images routinely used for knee imaging at 7T.Acknowledgements
The authors acknowledge assistance form study coordinators and MR technologists.References
1. Magee T, Williams D. 3.0-T MRI of Meniscal Tears. Am. J. Roentgenol. 2006;187:371–375. doi: 10.2214/AJR.05.0487.
2. Phelan N, Rowland P, Galvin R, O’Byrne JM. A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surgery, Sport. Traumatol. Arthrosc. 2016;24:1525–1539. doi: 10.1007/s00167-015-3861-8.
3. Chebrolu VV, Kollasch P, Howe B, Frick M, Carlson S, Spence D, Amrami K. Improving the Conspicuity of Meniscal Tears in Knee MRI at 3T and 7T. In: Proceedings 27th Scientific Meeting, International Society for Magnetic Resonance in Medicine. Montréal, QC, Canada; 2019. p. 1397.
Figures