2794
Quantitative evaluation of compressed nerve roots treated by PETD in lumbosacral radiculopathy using diffusion tensor imaging1The First Affiliated Hospital of Nanjing Medical University, Nanjing, China, 2GE Healthcare, MR Research, Beijing, P.R. China, Beijing, China
Synopsis
In this study, we aim to investigate if diffusion tensor imaging can clinically evaluate lumbosacral radiculopathy before and after percutaneous transforaminal endoscopic discectomy. By measuring 66 patients pre- and post-operatively, we found the FA values at the proximal sub-regions (subarticular zone) are more effective and had a significant correlation with clinical symptoms. Besides, both located in the proximal sub-regions, the abnormal parts of DTT visualized nerves coincided with the changes of the FA values in compressed nerves before and after surgery. Therefore, in lumbosacral radiculopathy, DTI is a potential tool for clinical evaluation before and after PETD surgery.
INTRODUCTION
The degeneration of compressed nerves causes the majority of clinical symptoms in lumbar disc hernia related lumbosacral radiculopathy1-3. The preoperative diagnosis and postoperative evaluation of lumbosacral radiculopathy are closely related to the microstructural changes along the compressed nerves. As can reflect the microscopically pathological changes of peripheral nerve noninvasively, DTI is suitable to provide quantitative information in lumbosacral radiculopathy compared to conventional MRI4-6. In this study, for further clinical application of DTI in lumbosacral radiculopathy, it is important to know, if quantitative DTI parameters could correlate with the clinical symptoms pre- and post-operatively.METHODS
Subjects:Sixty-six patients (36 men, age: 42.1±15.4 range 16-70 years old; 30 women, age: 43.5±13.7 range 20-67 years old) were recruited to this study. MR scanning and JOA scoring were applied before and 3-month after surgery for each patient. All patients received conventional percutaneous transforaminal endoscopic discectomy (PETD) by the same surgeon.
DTI protocol:
All MRI scans were performed using a 3-T scanner (Discovery 750w, GE Healthcare) equipped with a 16-channel body coil. An echo-planar imaging DTI sequence was performed for L4 to S1 nerve roots imaging with the following parameters: motion probing gradients applied in 11 directions; TR, 6000 ms; TE, 80 ms; FOV, 420 mm × 420 mm; matrix, 96 × 128; actual voxel size, 4.38 mm × 3.28 mm × 4.0 mm; calculated voxel size, 1.64 mm × 1.64 mm × 4.0 mm; NEX, 4; slice count, 60; slice thickness, 4mm; slice gap, 0; b-value, 800s/mm2. Array spatial sensitivity encoding technique (ASSET) was applied in DTI for scan acceleration. The corresponding scan time was 7 minutes, 24 seconds.
Data analysis:
All DTI data were processed with a DTI post-processing software embedded into the Functool platform at a GE workstation (Advantage workstation 4.6; GE Medical Systems). SPSS software (version 18.0.0; SPSS Inc) was used to perform statistical analysis. The embedded paired t-test toolbox was applied to compare the FA and ADC values of nerves between the symptomatic and asymptomatic sides at three sub-regions pre- and post-operatively. The correlation of clinical JOA scores and FA/ADC values of nerves was analyzed by correlation coefficient test. Multiple linear regression analysis was conducted to estimate the independent association between the clinical JOA scores and the FA/ADC values of nerves at these three sub-regions. The significant threshold for data analysis was set at p=0.05.
RESULTS
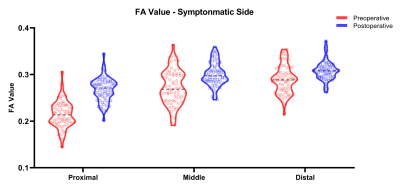
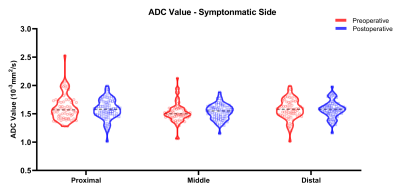
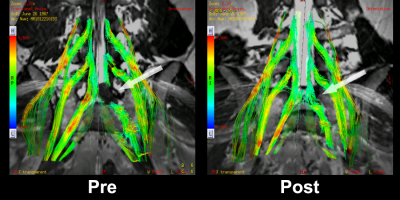
The postoperative FA values of compressed nerves were significantly higher compared with preoperative FA values at all sub-regions (p<0.001, Fig 1). There were no significant differences between pre- and post-operative ADC values at all sub-regions (Fig 2). The visual abnormalities of tractography mainly (64 cases, 96.9%) located in the proximal sub-region of compressed nerves. The improvement of compressed nerve tractography showed visually after surgery (Fig 3). Multiple linear regression analysis identified significant associations between the clinical JOA scores and the FA values of the compressed nerves at the proximal and distal sub-regions (JOA-s: R2 = 0.362; JOA-c: R2 = 0.442; total of JOA: R2 = 0.452). Furthermore, as independent variables, the proximal FA values made the greatest contribution (JOA-s: ΔR2 = 0.311; JOA-c: ΔR2 = 0.408; total of JOA: ΔR2 = 0.407) to the multiple linear regression model (Fig 4). There was no significant correlation between JOA scores and the ADC values of compressed nerves at all sub-regions.DISCUSSION
In this study, the results indicated that the FA values calculated at the proximal sub-regions (subarticular zone) are more effective in evaluating the lumbar nerve roots pre- and post-operatively. We also found that each separate parameter of JOA score and a total JOA score had a significant correlation with the FA values of compressed nerves at proximal sub-regions. Besides, both located in the proximal sub-regions, the abnormal parts of DTT visualized nerves coincided with the changes of the FA values in compressed nerves before and after surgery in this study. Hence, by DTI parameter FA values, the compressed lumbar nerves can be quantitatively evaluated and intuitively visualized in clinical practice before and after surgery.CONCLUSION
As can quantitatively reflect clinical symptoms and intuitively perform nerve roots tractograhy in lumbar disc hernia related lumbosacral radiculopathy, DTI is a potential tool for clinical evaluation before and after PETD surgery.Acknowledgements
No acknowledgement found.References
1. Hou SX, Tang JG, Chen HS, Chen J. Chronic inflammation and compression of the dorsal root contribute to sciatica induced by the intervertebral disc herniation in rats. PAIN 2003;105:255-264
2. Garfin SR, Rydevik B, Lind B, Massie J. Spinal nerve root compression. Spine (Phila Pa 1976) 1995;20:1810-1820
3. Barr K. Electrodiagnosis of Lumbar Radiculopathy. PHYS MED REH CLIN N 2013;24:79-91
4. Mürtz P, Kaschner M, Lakghomi A, et al. Diffusion-weighted MR neurography of the brachial and lumbosacral plexus: 3.0T versus 1.5T imaging. EUR J RADIOL 2015;84:696-702
5. Sun C, Hou Z, Hong G, Wan Q, Li X. In vivo evaluation of sciatic nerve crush injury using diffusion tensor imaging: correlation with nerve function and histology. J Comput Assist Tomogr 2014;38:790-796
6. Oikawa Y, Eguchi Y, Inoue G, et al. Diffusion tensor imaging of lumbar spinal nerve in subjects with degenerative lumbar disorders. MAGN RESON IMAGING 2015;33:956-961
Figures