2790
Evaluating the preoperative diagnose of lumbosacral radiculopathy using diffusion tensor imaging and tractography1The First Affiliated Hospital of Nanjing Medical University, Nanjing, China, 2GE Healthcare, MR Research, Beijing, P.R. China, Beijing, China
Synopsis
The aim of this study is mainly to explore the pre-diagnosis value of DTI technology applied to lumbosacral radiculopathy (LSR). By measuring 80 patients with unilateral disc related lumbosacral nerve root compression, we found that DTI technology combined with tractography not only could identify the type of disc herniation, assess the degree of nerve root damage, but also confirm the responsible nerve root. Therefore, we can demonstrate that DTI combined with tractography can improve the diagnosis rate of LSR and reduce iatrogenic injury.
Introduction
Lumbosacral radiculopathy used to assist diagnosis with conventional MR, which of prevalence is approximately 3% to 5%, distributed equally in men and women.1-3 Lumbar intervertebral disc protrusion is the most common cause underlying nerve root irritation and subsequent radiculopathy.4-6Conventional MRI cannot selectively visualize peripheral nerves or quantify the severity of nerve injury.7 DTI technique can reconstruct the fiber bundle shape by detecting the movement of water molecules, and react to the nerve root function by the change of FA value.8-10 However, it remains unknown if DTI combined with tractography is feasible to evaluate the nerve fibers in lumbosacral radiculopathy.Our research is mainly to explore the pre-diagnosis value of DTI technology applied to LSR, including the judgment of the type of disc herniation, the application of DTT images and the diagnostic efficacy of responsible nerve roots.Methods
Subjects:This study enrolled 80 patients (44males, 36 females, mean age 45.1±11.4 years) with LSR due to lumbar disc herniation. Conventional MRI and DTI with tractography were performed. All patients underwent endoscopic nerve root lysis and recorded the positional relationship between the intervertebral disc and the nucleus pulposus to verify the results of DTI. DTI Protocol3D MR sequence used Field of view (FOV) 32 cm × 32 cm, matrix 320 × 320, layer thickness 1 mm, layer spacing 0, standard voxel size 1 mm × 1 mm × 1 mm, scanning time 4 min 20 s..The DTI sequence scan used an 8-channel abdominal surface receiving coil using a single-shot spin echo-echo plane image (SS-SE-EPI). DTI parameters of axial lumbosacral nerve roots: diffusion sensitive gradients took 11 different directions, diffusion weighting coefficients (b) were 0 and 800 s/mm2, TR 7000.0ms, TE 90.0ms, FOV 42 cm × 42 cm, matrix 128 ×96, layer number 30, layer thickness 5 mm, layer spacing 0, standard voxel size 3.28 mm × 4.38 mm × 5.00 mm, measuring voxel size 1.64 mm × 1.64 mm × 5.00 mm, excitation times 4 times, scanning time 6 Min 37 s. Data analysis Data analyses were performed with IBM SPSS Statistics version 22 software. A unidirectional ordered R*C cross-tabulation was drawn, then comparison of the degree of nerve root damage between different protruding types by nonparametric test was conducted. Nemenyi test was used for pairwise comparison. The diagnostic ROC curve for lumbosacral radiculopathy of DTI and conventional MR was drawn. ROC curve comparison analysis was performed with SAS version 9.4 software. The inter- intra-observer variation was analyzed with Pearson correlation coefficients. A threshold of p < 0.05 was considered significant.Results
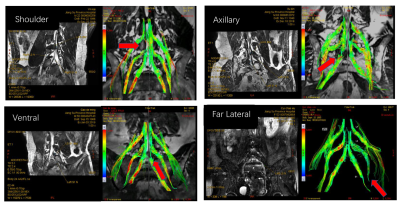
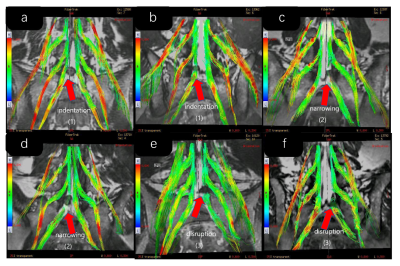
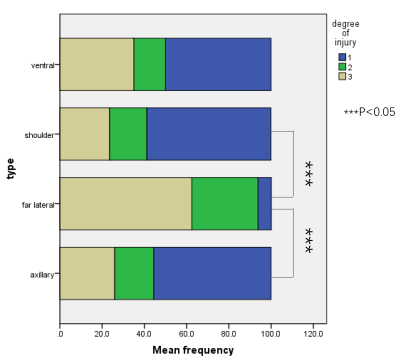
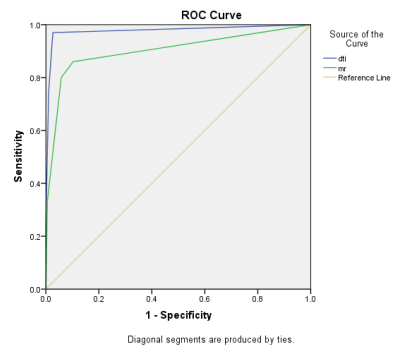
After verification during operation, the accuracy of DTI for the protruding type is 91.25% for all patients. DTI could accurately describe the anatomical relationship between the protruding nucleus pulposus and the nerve root, including shoulder type, axillary type, ventral type, and far lateral type (Figure 1). In all patients, DTT could clearly show the morphology of fibrous nerve bundles with a quantitative assessment of DTI derived FA values (Figure2). A unidirectional ordered R*C cross-tabulation was drawn and Figure 3 showed that the nerve roots of the far lateral protrusion type are more damaged than the shoulder type and the axillary type. ROC curve at all nerve roots was illustrated in Figure 4 and Table 2. The area under the curve of DTI was 0.978, and the area under the curve of MR was 0.902.Discussion
Our research proves that DTI does have a unique advantage in clinical diagnosis of LSR. Fractional anisotropy (FA) is a quantitative diffusion value that reflects the directionality of molecular diffusion.9,10 We found a difference of clinical manifestations in patients with different protrusion types. We differentiate the degree of damage to statistics, and found that the far lateral type had the serious damage degree (Figure 3), agreed with the clinical results. The reason may be explained that the dorsal root ganglion is compressed or the nerve root is moved up and close to the lower edge of the superior pedicle to form an extrusion.8 The determination of the responsible nerve root is conducive to the accurate diagnosis of LSR and reducing iatrogenic injury. Hence, the clinical diagnosis of patients that suffer from lumbar intervertebral disc related radiculopathy can be quantitatively confirmed by DTI combined with tractography.Conclusion
In conclusion, DTI combined with DTT images have advantages in the diagnosis of LSR, including the definition of disc herniation, the degree of nerve root damage and the determination of responsible nerve root.Acknowledgements
No acknowledgement found.References
1. Heliovaara, M., Knekt, P. & Aromaa, A. Incidence and risk factors of herniated lumbar intervertebral disc or sciatica leading to hospitalization. Journal of chronic diseases 40, 251-258, 1987.
2. Weiner, B. K. & Patel, R. The accuracy of MRI in the detection of lumbar disc containment. Journal of orthopaedic surgery and research 3, 46, 2008.
3. Carrino, J. A. et al. Lumbar spine: reliability of MR imaging findings. Radiology 250, 161-170, 2009.
4. Van Boxem, K. et al. 11. Lumbosacral radicular pain. Pain practice : the official journal of World Institute of Pain 10, 339-358, 2010.
5. Schafer, A., Hall, T. & Briffa, K. Classification of low back-related leg pain--a proposed patho-mechanism-based approach. Manual therapy 14, 222-230, 2009.
6. Mondelli, M. et al. Clinical findings and electrodiagnostic testing in 108 consecutive cases of lumbosacral radiculopathy due to herniated disc. Neurophysiologie clinique = Clinical neurophysiology 43, 205-215, 2013.
7. Kimura, S., Steinbach, G. C., Watenpaugh, D. E. & Hargens, A. R. Lumbar spine disc height and curvature responses to an axial load generated by a compression device compatible with magnetic resonance imaging. Spine 26, 2596-2600, 2001.
8. Mukherjee, P., Chung, S. W., Berman, J. I., Hess, C. P. & Henry, R. G. Diffusion tensor MR imaging and fiber tractography: technical considerations. AJNR. American journal of neuroradiology 29, 843-852, 2008.
9. Khalil, C. et al. Tractography of peripheral nerves and skeletal muscles. European journal of radiology 76, 391-397, 2010.
10. Andreisek, G., White, L. M., Kassner, A. & Sussman, M. S. Evaluation of diffusion tensor imaging and fiber tractography of the median nerve: preliminary results on intrasubject variability and precision of measurements. AJR. American journal of roentgenology 194, W65-72, 2010.
Figures