2782
Bone Imaging in Musculoskeletal Trauma with Zero Echo-Time MRI
Ryan E Breighner1, Matthew F Koff1, and Hollis G Potter1
1Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States
1Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States
Synopsis
Zero Echo Time (ZTE) MRI yields positive contrast for bone visualization using MRI. The present study highlights cases in which ZTE provides additional diagnostic information in the context of orthopedic trauma. The presented cases are ones in which MRI was deemed necessary for the evaluation of ligament, tendon, or nerve integrity and ZTE was added to aid in the assessment of fractures. In conjunction with our prior work, this study demonstrates that ZTE MRI provides additional diagnostic information in musculoskeletal MRI, specifically in the context of joint trauma.
Introduction
Traumatic injuries to the musculoskeletal system frequently feature complex involvement of osseous and soft tissues. Fractures near joints raise clinical concerns of ligament ruptures and avulsions as well as disruption of tendon insertions near the site of fracture. Additionally, complex fractures may involve neurovascular structures traversing the fracture site. In order to comprehensively evaluate these injuries, accurate imaging of both bone and soft tissue is necessary. Conventional MRI pulse sequences typically render bone as void owing to locally reduced water content (20-40% bound water) and concomitant rapid transverse tissue relaxation time (T2* ≈ 270μs) in cortical bone.1,2 Newer pulse sequences, such as Zero Echo Time (ZTE) MRI, are capable of acquiring image data immediately (8μs) after excitation, yielding a detectable contrast gradient through cortical bone and facilitating ready differentiation of bone from other short T2 tissue species.In this study, we evaluated complex cases in which concurrent imaging of soft tissue and bone was obtained by augmenting standard-of-care (SOC) MRI with ZTE. The added utility of ZTE MRI in the context of these musculoskeletal traumas is readily apparent in images and derived 3D reconstructions.
Methods
Informed consent was obtained for ZTE imaging at physicians’ requests as part of a larger, IRB approved study. Following institutional SOC MRI pulse sequences, a ZTE acquisition was performed, adding approx. 5-7 minutes to total exam time. To date, over 600 ZTE scans have been performed at our institution. Acquisition parameters for ZTE imaging were as follows: TR: 300ms, flip angle: 1°, receiver bandwidth: ±62.5 kHz, matrix size: 320, slice thickness: 0.8-1.5 mm, scan time: 4-6 min, field-of-view (FOV): 10-32cm. Commercially available coils were utilized for all scans (Invivo, Gainesville, FL or GE Healthcare, Waukesha, WI). Coil selection and field of view size varied with patient size and anatomy of interest. All scans were performed on clinical 3T MRI scanners (Signa Premier and Discovery MR750, GE Healthcare).Results
Figures 1-4 are examples of ZTE images and ZTE-based volume renderings where ZTE may add diagnostic utility to MRI examinations in the context of musculoskeletal trauma. Figure 1 shows a displaced, multi-fragment fracture of the proximal radial head (highlighted in blue). The ZTE-derived volume rendering provides clear visualization of the extent of the fracture and the degree of fragment displacement. Figure 2 demonstrates a more subtle fracture of the proximal radial head. Side-by-side comparison with proton density-weighted (PDW) MRI demonstrates greater conspicuity in ZTE images. MRI was principally required in both cases to assess the ulnar nerve and collateral ligaments of the elbow.Figure 3 shows ZTE MRI of fractures of the 2nd-4th metatarsals, secondary to bimalleolar fractures of the ankle (not shown). The fracture to the 2nd metatarsal is minimally displaced and not apparent on PDW images (C). Figure 4 shows a shoulder fracture wherein a significant portion of supraspinatus tendon footprint was avulsed and retracted between the humeral head and acromion (B).
Discussion
Musculoskeletal traumatic injuries, like those presented here, require evaluation of osseous and soft tissue. As shown in the above cases, a ZTE MRI acquisition complements a SOC MRI examination to achieve these goals and aid in the detection of clinically-relevant osseous details. Concurrent acquisition of bony morphology with nearly identical patient positioning enables the radiologist to evaluate bone and soft tissue injuries in the same joint orientation and position without image registration. ZTE MRI is not conducive to imaging near arthroplasty or osteosynthesis hardware as it is susceptible to metal artifact.Our prior work3-5 has shown appreciable agreement between ZTE MRI and CT imaging, and that ZTE may serve as a viable substitute in certain cases. In addition, the present cases demonstrate additional utility of MRI of musculoskeletal trauma by providing a means to acquire osseous morphology during the same exam. This is not only beneficial diagnostically, it may save the patient the time and financial cost of a second imaging appointment and may mitigate ionizing radiation dose attendant to CT examination.
Acknowledgements
HSS maintains an institutional research agreement with GE Healthcare.References
- Chen et al. 2015. NMR Biomed 28(12).
- Techawiboonwong et al. 2008. Radiology 248(3).
- Breighner et al. 2019, AJSM (epub, ahead of print)
- Breighner et al. 2018, Radiology 286(3).
- Argentieri et al. 2017, Spine 43(13).
Figures
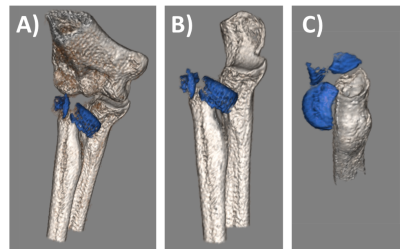
Figure 1. ZTE-derived
segmented volume-renderings. 25 y/o male, fracture of the radial head (fragments
shown in blue). A) Anteromedial aspect. B) Anterior aspect, humerus removed. C)
Superoposterior view, humerus and ulna removed.
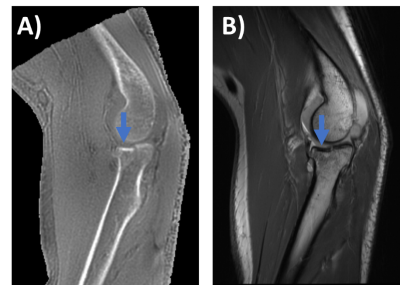
Figure
2. Sagittal ZTE (A) and PDW MRI (B) of depressed radial head fracture in 29 y/o
male. Though discernable in both MR sequences, the fracture and step-off is more
conspicuous in ZTE as only subchondral bone is rendered and not cartilage.
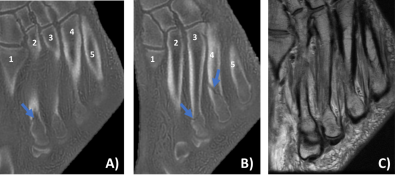
Figure 3. Coronal ZTE
(A, B) and PDW MRI (C) of the midfoot (62 y/o male) showing fractures of the
distal 2nd (A) and 3rd and 4th (B) metatarsals
(arrows). Fracture to the 2nd metacarpal is not apparent in PDW
images.
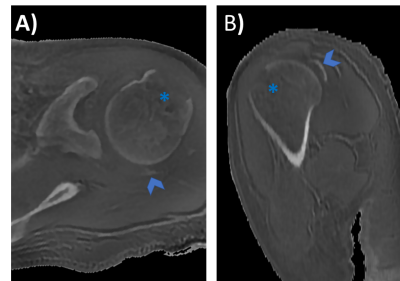
Figure 4. ZTE axial
(A) and sagittal (B) images showing a shoulder fracture (27 y/o female) with appreciable
avulsion (asterisks) and retraction of the supraspinatus footprint (chevrons).