2766
The feasibility study of 3D adiabatic inversion recovery prepared ultrashort TE Cones sequence in the evaluation of osteoporosis1Department of Radiology, The Fifth Affiliated Hospital of Sun Yat-Sen University, Guangdong, China, 2University of California, San Diego, California, San Diego, CA, United States, 3The Tird Affiliated Hospital of Southern Medical University, Guangdong, China, 4MR Research, GE Healthcare, Beijing, China
Synopsis
The current study aims to assess the feasibility of proton density (PD) in the lumbar using 3D adiabatic inversion recovery prepared ultrashort TE cones (3D IR‐UTE‐Cones) sequence. In addition, the latent associations between the PD and BMD, age, gender, the oswestry disability index (ODI) were evaluated, respectively. It was concluded that proton density of trabecular bone can be applied in lumbar. Moreover, the proton density of lumbar were observed to correlate with BMD, age and ODI, which need further study to clarify this topic.
Introduction
Osteoporosis is a systemic skeletal disease, it is characterized by low bone mass, poor structure, and increased risk of fracture1. Trabecular bone is highly responsive to metabolic stimuli and has a turnover rate ~8 times higher than that of cortical bone, making it a main index for detecting bone loss in early osteoporosis (OP)2. In this study, we utilized a broadband adiabatic inversion recovery prepared 3D UTE cones (3D IR‐UTE‐cones) sequence3 to investigate the characterizations of trabecular bone in human lumbar and to further evaluate the correlations between lumbar PD and BMD, age, gender, ODI, respectively, in osteoporosis patients.Methods
10 osteoporosis patients (age 48±12 years, age range 40-76 years) were recruited. All patients underwent 3D IR‐UTE‐cones sequence of lumbar on a 3.0T MR station (Signa, Pioneer, GE Healthcare). A phantom with a T2*around 0.34 ms was placed between the patients and the spine coil during scanning to serve as a reference to calibrate the proton density of trabecular bone3. The UTE sequence parameters were as follows: TR/TI = 150/64 ms, TE = 0.032 ms, flip angle = 18°, FOV = 30cm × 30cm, matrix = 140 × 140, oversampling factor = 2, and scan time = 10 min. QCT examinations of the lumbar region in the supine position were performed on a 64-detector CT scanner (Aquilion 64, Toshiba, Tokyo, Japan) for each subject. The QCT images were acquired using the following parameters: tube voltage, 120 kVp; tube current, 150 mA; rotation time,500 msec; slice thickness, 1 mm; and field of view (FOV), 50cm × 50 cm. Regions of interest (ROIs) were placed in the vertebral body, avoiding cortical bone. Mean lumbar PD was computed for each subject by averaging the PD measurements from three vertebrae (L3–L5). Pearson correlation analysis was performed to calculate the correlations between lumbar PD and BMD, age, gender, ODI, respectively, in osteoporosis patients. A value of P < 0.05 was considered as a statistically significant.Results
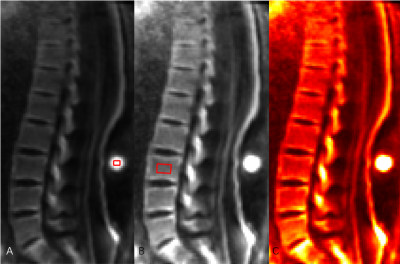
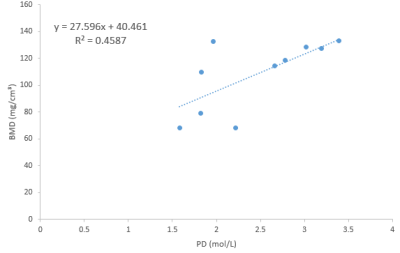
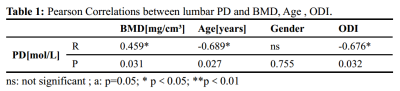
The lumbar UTE images of each participants were successfully acquired in our study (Figure 1). The lumbar PD showed a moderate positive correlation with BMD (r = 0.459, P < 0.05) (Figure 2). In addition, our results demonstrated that the lumbar PD is negatively correlated with age (r = -0.689, P < 0.05) and ODI (r = -0.676, P < 0.05), while had no association with gender. The results were summarized in table 1.Discussion and Conclusion
To our best knowledge, this is a preliminary study of applying PD measured by IR-UTE MRI in lumbar. It is concluded that PD of the lumbar can be achieved by using a clinical 3.0T MRI with a 10 mins IR-UTE sequence. The decreased PD in the osteoporotic lumbar vertebrae could be partly explained by the decreased BMD. Accurate evaluation of trabecular bone is worthwhile, because most osteoporotic fractures occur at locations with rich trabecular bone4. It is feasible that PD can be applied in the diagnosis of osteoporosis using IR-UTE. Overall, it is supposed that the IR-UTE based imaging biomarkers could be utilized to predict compression fracture of lumbar.Acknowledgements
No acknowledgement found.References
[1] NIH Consensus Development Panel on Osteoporosis Prevention D, Jama TJ. Osteoporosis Prevention, Diagnosis, and Therapy. 2001;285(6):785-795.
[2] Majumdar S. Magnetic resonance imaging of trabecular bone structure. Top Magn Reson Imaging. 2002;13:323–334.
[3] Ma YJ, Chen Y, Li L, Cai Z, Wei Z, Jerban S, Jang H, Chang EY, Du J. Trabecular bone imaging using a 3D adiabatic inversion recovery prepared ultrashort TE Cones sequence at 3T. Magnetic resonance in medicine. 2019;00:1–12.
[4] Wehrli FW, Song HK, Saha PK, Wright AC. Quantitative MRI for the assessment of bone structure and function. NMR Biomed. 2006;19:731–764.
Figures