2726
Longitudinal Analysis of Knee Articular Cartilage in Collegiate Basketball Players and Swimmers: Preliminary Results1Stanford University, Stanford, CA, United States, 2Santa Clara University, Santa Clara, CA, United States, 3University of California San Francisco, San Francisco, CA, United States, 4Hospital for Special Surgery, New York, NY, United States
Synopsis
Basketball players place high loads on their knee joints that can lead to chronic knee injuries. In this study, we used advanced MRI methods and a cluster analysis to longitudinally study cartilage structure and potential early degenerative changes in Division 1 (D1) basketball players and swimmers. Pre-season and post-season quantitative results indicate an increase in T2 and T1p relaxation times in the central compartment of the femoral cartilage in the basketball players compared to the swimmers. The results of this study suggest that microstructural changes in knee cartilage can occur in one season of D1 college play.
Introduction
Jumping and impact athletes put extra mechanical stress on their joints which can lead to chronic knee injuries. In professional basketball players, patellofemoral injuries are the most common cause of missed games1. Advanced MRI methods offer a way to non-invasively study early changes in knee articular cartilage2 and a player's overall risk of degenerative disease progression. In this multicenter study, we use advanced quantitative MRI metrics of T1ρ and T2 to longitudinally study early cartilage changes in Division 1 (D1) basketball players compared with D1 swimmers. The aim of this study is to investigate the effect of one season of (D1) basketball play on the imaging findings of an athlete's articular cartilage microstructure.Methods
In this multicenter longitudinal study, National Collegiate Athletic Association (NCAA) athletes underwent an MRI before and after their NCAA season using a GE 3T SIGNA Premier scanner (GE Healthcare, Milwaukee, WI, USA) and a 16-channel flexible phased-array, receive-only coil (NeoCoil, Pewaukee, WI, USA). The study included 14 D1 basketball players (8 female) and 4 D1 swimmers (3 female). Athletes were scanned using an MRI protocol (Table 1) that included a 3D sagittal combined T1ρ/T2 magnetization-prepared angle-modulated portioned k-space spoiled gradient echo snapshots (MAPSS) sequence3. T2 and T1ρ relaxation time maps were computed using a mono-exponential fit of signal data acquired at various echo/spin-lock (TE/TSL) times (Table 1). Subsequently, we utilized a cluster analysis method4 to identify differences in 2D T1p and T2 relaxation mapping over time in basketball players and swimmers. Within the cluster analysis, we identified clusters or contiguous pixels with a size great than 12.4 mm2 where T2 and T1p increases were greater than two standard deviations above the changes seen in the comparison population of swimmers. Projection maps were subtracted (post-season) – (pre-season) to create difference maps that we used to identify clusters in the basketball players based off of a predetermined intensity and size threshold calculated off of the swimmer’s average changes in T2 and T1p relaxation times. The intensity and size threshold were 3.42ms and 15 pixels for T2 and 5.1265ms and 15 pixels for T1p. To calculate the difference in T1ρ and T2 relaxation times during the season the (post-season) – (pre-season) results were calculated. A generalized linear model was used to compare the T1ρ and T2 relaxation times of the basketball players to those of the swimmers.Results
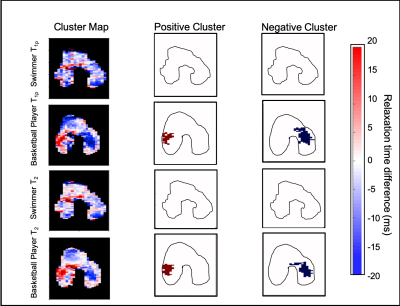
A summary of NCAA pre-season and post-season T2 and T1p relaxation times for patellar and femoral cartilage is in Figure 1. Basketball players showed significantly less of a decrease in relaxation times during their NCAA season in the anterior and central compartments of their femoral cartilage compared to the swimmers. The basketball players had significantly less of a decrease in the medial anterior compartment in T1p (p = 0.0233) and T2 (p = 0.0253) and lateral anterior compartment in T1p (p = 0.005) and T2 (p < 0.001) of their femoral cartilage (Figure 2). With regards to the cluster analysis, the percentage of cluster area with significant positive clusters in the femoral cartilage was significantly higher in the basketball players compared to the swimmers for T2 (p = 0.009) and for T1p (p = 0.021) (Figure 3). The cluster analysis of the femoral cartilage showed that athletes with significant clusters had a positive cluster in the medial central compartment and a negative cluster in the lateral central compartment or vice versa depending on the athlete (Figure 4).Discussion
Generally, T2 and T1p relaxation times are affected by hydration levels in the cartilage and an increase in the relaxation times are respectively associated with collagen matrix change or a loss of cartilage proteoglycan content5. During the course of the NCAA season both populations had a general decrease in relaxation times in their femoral cartilage. The larger decrease in T1p and T2 relaxation times in the swimmers compared to the basketball players may indicate that swimming has less of a negative impact on joint health compared to basketball. This could indicate that the swimmer’s off-season puts more stress on their joints due to increased dry land workouts (weight-lifting and running) and that their in-season loading is beneficial to the swimmer's cartilage health. Our cluster analysis showed significant positive clusters in one side of the central (weight-bearing) compartment of their femoral cartilage which indicated that players may placing more load on one side of their knee compared to the other.Conclusion
Knowledge of injury patterns can help to guide treatments and inform strategies for keeping athletes healthy. It is evident based on the significant change in quantitative values over the course of the season that sports can impact the health of a player’s articular cartilage over a relatively short period of time. This work demonstrates the immediate effects of a season of play and possible positive or negative effects that may occur during an athlete’s season and can be used to inform strategies related to training and rest across a season. Future studies will focus first on the difference between post-season quantitative MR metrics compared with the following pre-season in order to measure the effect of the off-season and later on 3 year longitudinal results.Acknowledgements
This work was funded by the NBA and GE Healthcare Orthopedics and Sports Medicine Collaboration.References
1. Drakos, M. C., Domb, B., Starkey, C., Callahan, L., & Allen, A. A. (2010). Injury in the national basketball association: a 17-year overview. Sports health, 2(4), 284–290. doi:10.1177/1941738109357303.
2. Disler DG, Recht MP, McCauley TR. MR imaging of articular cartilage. Skeletal Radiol 2000; 29:367-377.
3. Li, X., Han, E. T., Busse, R. F., & Majumdar, S. (2008). In vivo T(1rho) mapping in cartilage using 3D magnetization-prepared angle-modulated partitioned k-space spoiled gradient echo snapshots (3D MAPSS). Magnetic resonance in medicine, 59(2), 298–307. doi:10.1002/mrm.21414.
4. Monu, U. D., Jordan, C. D., Samuelson, B. L., Hargreaves, B. A., Gold, G. E., & McWalter, E. J. (2017). Cluster analysis of quantitative MRI T2 and T1ρ relaxation times of cartilage identifies differences between healthy and ACL-injured individuals at 3T. Osteoarthritis and cartilage, 25(4), 513–520. doi:10.1016/j.joca.2016.09.015
5. Choi, J. A., & Gold, G. E. (2011). MR imaging of articular cartilage physiology. Magnetic resonance imaging clinics of North America, 19(2), 249–282. doi:10.1016/j.mric.2011.02.010.
6. Meeuwisse WH, Sellmer R, Hagel BE. Rates and risks of injury during intercollegiate basketball. Am J Sports Med 2003;31:379–85. 10.1177/03635465030310030901.
7. Cumps, E., Verhagen, E., & Meeusen, R. (2007). Prospective epidemiological study of basketball injuries during one competitive season: ankle sprains and overuse knee injuries. Journal of sports science & medicine, 6(2), 204–211.
Figures
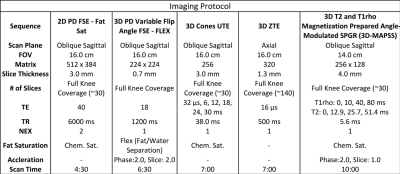
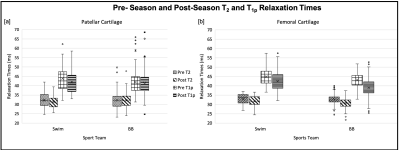
Figure 1: [a] Across the patellar cartilage there was a trend of decreasing T2 and T1p relaxation times in the swimmers while the basketball players showed more consistent values. [b] The femoral cartilage showed a similar trend in the patellar cartilage of decreasing T2 and T1p relaxation times over the course of the NCAA season.
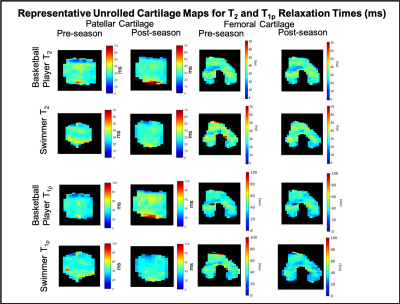
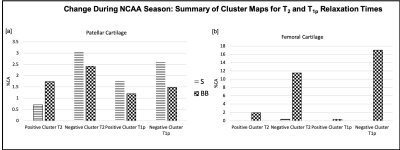
Figure 3: [a] In the patellar cartilage there was a trend of more positive clusters with T2 relaxation times in the basketball players compared to the swimmers. Swimmers had a trend of more negative clusters with both T2 and T1p in the swimmers compared to the basketball players. [b] In the femoral cartilage basketball players showed significantly more positive and negative clusters than the swimmers for T2 (p = 0.009) and for T1p (p = 0.021).