2681
Evaluation of Kinematics and Image Quality of Thoracic Outlet during Humeral Elevation in Normal Volunteers Using 3D-MRI with Compressed Sensing1Department of Radiology, Keio University School of Medicine, Tokyo, Japan, 2Department of Radiology, St. Luke's International Hospital, Tokyo, Japan, 3Department of Intelligent Image Information, Gifu University School of Medicine, Gifu, Japan, 4Department of Orthopaedic Surgery, St. Luke's International Hospital, Tokyo, Japan
Synopsis
We performed 3D-MR imaging with compressed sensing on the thoracic outlet of 23 normal volunteers, comparing it with conventional 2D-MR imaging. The image quality score of 3D-PDWI with compressed sensing was significantly lower than that of 2D-PDWI. However, no significant difference in the image quality score of MRA with compressed sensing due to arm position was demonstrated. Subclavian arterial stenosis during humeral elevation was shown in 30.4% of asymptomatic subjects without gender predominance. 3D-MR imaging using compressed sensing enables us to evaluate the kinematics of the thoracic outlet, and may contribute to the diagnosis of TOS in clinical settings.
Introduction
Due to a lack of objecting reporting criteria, the diagnosis of thoracic outlet syndrome (TOS) is difficult. However, the contribution of MRI to the depiction of vascular and nerve compression in the thoracic outlet has been outlined 1. Previous studies using 2D-MR imaging have shown the presence of the stenosis of thoracic outlet even in asymptomatic cases 2, but its pathophysiology and frequency have been unclear. The purpose of this study is; 1) to establish an optimal 3D-MR sequence for the thoracic outlet that can be applied in clinical settings, comparing it with conventional 2D MR sequence, 2) to clarify the frequency and pathophysiology of stenosis of subclavian vessels and brachial plexus in normal volunteers.Materials & Methods
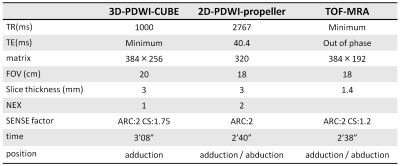
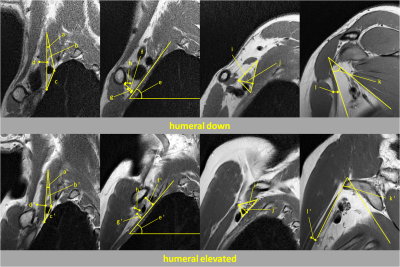
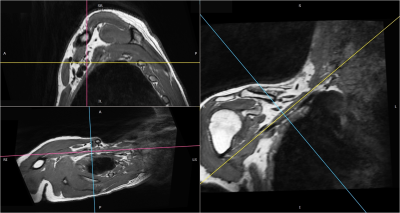
The thoracic outlet of dominant arm in 23 normal volunteers (13 men, 10 female. Mean age: 31.6 ± 8.7 years) were imaged using a GE 750w 3.0T MRI scanner (GE Healthcare, Milwaukee, WI) with 16 channel Flex L-coil. 2D-PDWI and TOF-MRA with compressed sensing were obtained with subject’s arms in adduction and in abduction. 3D-PDWI with compressed sensing was obtained with arms in adduction. Detailed MRI protocol was shown in Figure 1. Qualitative and quantitative analyses of the thoracic outlet were performed by two board-certified radiologists with subspecialization in musculoskeletal radiology independently. 3D-PDWI and 2D-PDWI were qualitatively graded for the delineation of anatomic structures. The presence or absence of stenosis of the subclavian vessels and brachial plexus was visually evaluated with MIP images of MR angiography. In quantitative analysis, we measured the thickness and the angle of the muscles or bones that form the thoracic outlet, the distance between them and the area of the thoracic outlet at the interscalene space, the costoclavicular space, and the retropectoralis minor space using 2D images, respectively as Figure 2. We calculated the reduction rate of those areas during humeral elevation. Then, oblique MPR images aligned with the brachial plexus were created from the original isotropic 3D images, and we measured each items on oblique MPR sections (Figure 3). The reproducibility of quantification was analyzed by the interclass correlation coefficients.Results
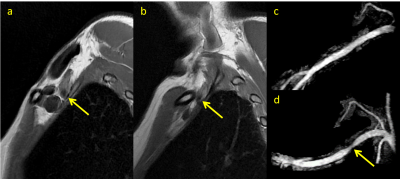
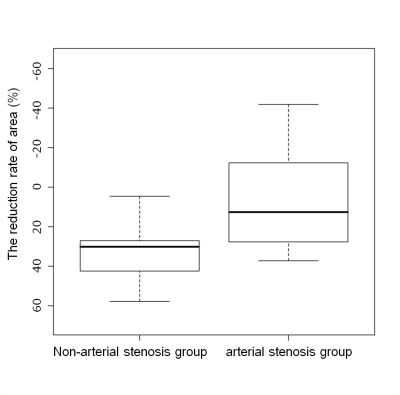
The image quality score of 3D-PDWI with compressed sensing was significantly lower than that of 2D-PDWI (3.91±0.95 vs 4.30±0.70, p<0.01). However, no significant difference in the image quality score of MRA due to arm position was demonstrated (4.52±0.66 vs 4.30±0.88, p=0.11). During humeral elevation, stenosis of the subclavian artery was visually shown in 7 subjects (30.4%) on 2D-PDWI and MRA. Of 7 subjects, 5 subjects are male and 2 subjects are female without gender predominance (38.5% vs. 20.0%, p= 0.41) (Figure 4). The reduction rate of area where the brachial plexus is surrounded by the subclavius muscle and the serratus anterior was significantly smaller in the arterial stenosis group compared with the non-arterial stenosis group (6.0% vs 29.0%, p=0.04) (Figure 5). The reduction rate in the angle between the first rib axis and horizontal tends to be small in female, although there was no significant difference (6.0% vs 11.0%, p=0.09). The angle between the pectoralis minor and the subscapularis in the retropectoralis minor space tends to be narrowed in the arterial stenosis group compared with the non-arterial stenosis group without significant difference (p=0.08). The intraclass correlation coefficient of the measurement in the costoclavicular space, retropectoralis minor space, and interscalene space was 0.720, 0.692, and 0.209 respectively.Conclusion
3D-MR imaging using compressed sensing enables us to evaluate the kinematics of the thoracic outlet, and may contribute to the diagnosis of TOS in clinical settings. We pay attention to the fact that subclavian arterial stenosis during humeral elevation was shown in 30.4% of asymptomatic subjects.Acknowledgements
No acknowledgement found.References
1. Demondion X, Bacqueville E, Paul C, et al. Thoracic outlet: assessment with MR imaging in asymptomatic and symptomatic populations. Radiology. 2003; 227:461-468.
2. Raptis CA, Sridhar S, Thompson RW, et al. Imaging of the Patient with Thoracic Outlet Syndrome. Radiographics. 2016; 36:984-1000.
Figures