2673
Assessment of infection after joint replacement by MAVRIC-SL MR imaging1Radiology, Toho University Sakura Medical Center, Sakura, Japan
Synopsis
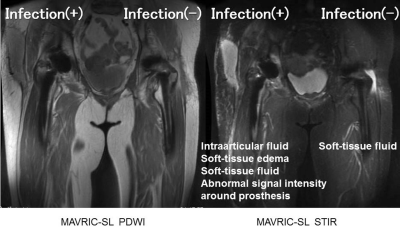
MAVRIC-SL sequence can improve the quality of images by decreasing metal artifacts and assess infection around prosthetic implants after joint replacement. Presence of intraarticular fluid is important for the diagnosis of infection after joint replacement. The risk of additional surgical intervention due to infection after joint replacement would be higher when there are more than three of the four findings including intraarticular fluid, soft-tissue edema, soft-tissue fluid, and abnormal signal intensity around prosthesis or both intraarticular fluid and abnormal signal intensity around prosthesis. MAVRIC-SL MR imaging must be a powerful tool for the assessment of infection around prosthetic joint implants.
Purpose
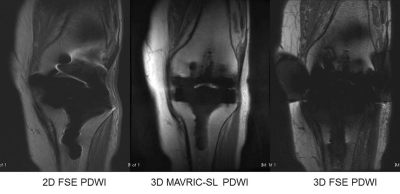
Implantation of joint prostheses is becoming increasingly common. Infection is the most devastating of prosthesis-related complications. Although conventional MR imaging has not been effective due to metal artifacts, MR imaging with metal-suppression sequences has recently been applied for assessment around prosthetic joint implants (Fig. 1) (1,2). The purpose of this study was to assess the value and findings of MR imaging with metal artifact suppression, multiacquisition variable-resonance image combination, slice encoding for metal artifact correction (MAVRIC-SL), for the assessment of infection after joint replacement.Materials and methods
28 joints in 24 patients (5 males, 19 females; mean age=75.9years; 16 hip, 10 knee, and two elbow joints) clinically suspected of periprosthetic infection after joint replacement were enrolled in this study. The patients all underwent joint MR imaging at 1.5T (Optima MR450W, GE healthcare). MAVRIC-SL PDWI (TR/TE:3800/6.3-7.7ms, slice thickness:4mm, NEX:0.5, FOV: 180x192-420x449mm) and MAVRIC-SL STIR (TR/TE:4500/6.3-7.8ms, slice thickness:4mm, NEX:0.5, FOV:180x192-420x490mm) were obtained. Total acquisition times of MAVRIC-SL PDWI and STIR sequence were around 6min. The quality of images (sharpness of bone contour, noise) of MAVRIC-SL PDWI and STIR was assessed using three-grading system (good, fair, and poor) by two certificated radiologists. Imaging findings including intraarticular fluid, soft-tissue edema, soft-tissue fluid, and abnormal signal intensity (SI) around prosthesis were also assessed. The finding of abnormal SI around prosthesis was determined as high signal intensity just around prosthetic implants in bone. Final diagnosis of infection after joint replacement was comprehensively determined based on swelling around joint, positive blood culture, elevation of serum C-reactive protein, and clinical course including improvement after antibiotic therapy or after surgical intervention. Odds ratio (OR) was calculated. P<0.05 indicated a statistically significant difference.Results
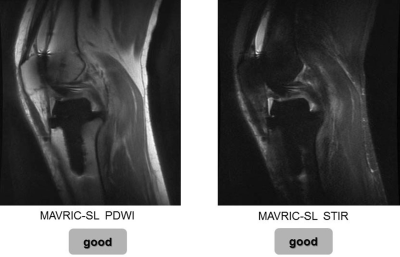
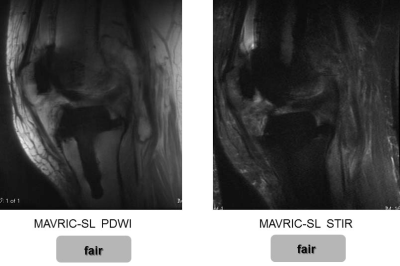
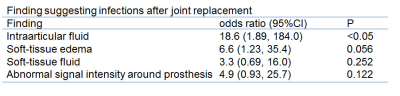
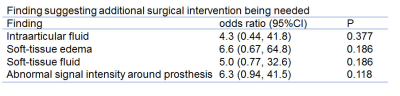
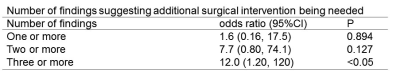
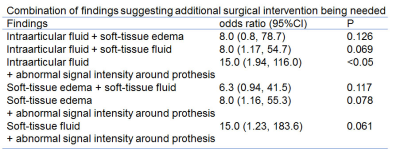
Twelve joints had periprosthetic infection, 2 had acute subcutaneous cellulitis, and 15 had no infection. In the 12 joints with periprosthetic infection and 2 with acute subcutaneous cellulitis, 7 (50%) needed additional surgical intervention including surgical debridement and implant removal. Regarding the image quality, 87% (20/23) showed good and 13% (3/23) showed fair on MAVRIC-SL PDWI, while 71% (20/28) showed good and 29% (8/28) showed fair on MAVRIC-SL STIR (Figs. 2 and 3). Overall, 20 joints had intraarticular fluid, 16 had soft-tissue edema, 12 had soft-tissue fluid, and 11 had abnormal SI around prosthesis. In the 14 joints with infection after joint replacement, 14 (100%) had intraarticular fluid, 12 (86%) had soft-tissue edema, 8 (57%) had soft-tissue fluid, and 6 (43%) had abnormal SI around prosthesis. In the 7 joints with additional surgical intervention, 7 (100%) had intraarticular fluid, 6 (86%) had soft-tissue edema, 5 (71%) had soft-tissue fluid, and 5 (71%) had abnormal SI around prosthesis. Regarding the finding suggesting infection after joint replacement, there was a statistically significant difference only in the presence of intraarticular fluid (OR:18.67, p<0.05) (Fig. 4). Regarding the finding suggesting additional surgical intervention being needed, there was no significant difference in the four findings (Fig. 5). However, there were significant differences when more than three of the four findings (OR:12.0, p<0.05) or the findings of intraarticular fluid and abnormal SI around prosthesis both were found (OR:15, p<0.05) (Figs. 6, 7 and 8).Discussion
The main findings in this study are that MR imaging with MAVRIC-SL can improve the quality of images by decreasing metal artifacts and assess around prosthetic implant after joint replacement. The quality of images was better on MAVRIC-SL PDWI than MAVRIC-SL STIR. MAVRIC-SL MR imaging disclosed that the presence of intraarticular fluid was important for the diagnosis of infection after joint replacement. The risk of additional surgical intervention including surgical debridement and implant removal would be higher when there were more than three of the four findings including intraarticular fluid, soft-tissue edema, soft-tissue fluid, and abnormal SI around prosthesis or both intraarticular fluid and abnormal SI around prosthesis.Generally, MR features of joint infection include synovitis, joint effusion, soft-tissue edema, bone edema, soft-tissue fluid collections, sinus tracts to the skin surface, bone destruction, and reactive lympheadenopathy (3). Our results disclosed that MARVRIC-SL MR imaging can depict these MR features even in the joints with prosthetic joint implants. MR imaging with MAVRIC-SL sequence must be a powerful tool for the assessment of osseous and soft-tissue complications related to prosthetic implants after joint replacement.
Our study did have some limitations, with the relatively low number of cases included being the first and most important of them. Second, we did not use contrast materials for the assessment of infection of bone and soft-tissue. However, the previous studies said that contrast materials are typically not necessary for the primary diagnosis of infection, but may be useful to define the fluid collections and sinus tracts (4).
Conclusion
MAVRIC-SL MR imaging is able to improve the quality of images by decreasing metal artifacts and assess infection around prosthetic implants after joint replacement. The presence of intraarticular fluid is important for the diagnosis of infection after joint replacement. The risk of additional surgical intervention would be higher when more than three of the four findings including intraarticular fluid, soft-tissue edema, soft-tissue fluid, and abnormal SI around prosthesis or both of intraarticular fluid and abnormal SI around prosthesis are found.Acknowledgements
No acknowledgement found.References
1. Susa M, et al. Novel MR imaging method-MAVRIC-for metal artifact suppression after joint replacement in musculoakeletal tumor patients. BMC musculoskelet disord 16:377, 2015
2. Talbot BS, et al. MR imaging with metal-suppression sequences for evaluation of total joint arthroplasty. RadioGraphics 36:209-225, 2016
3. Friz J, et al. MR imaging of hip arthroplasty implants. RadiGraphics 34:E106-E132, 2014
4. Koff MF, et al. Magnetic resonance imaging near orthopaedic hardware. J Magn Reson Imaging 46(1):24-39, 2017
Figures