2623
Post-treatment recovery of perfusion-related diffusion in the fatty liver of type 2 diabetes mellitus: an IVIM-DWI study1Department of Radiology, Henan Provincial People’s Hospital, Zhengzhou, China, 2MR Collaboration, Siemens Healthcare Ltd, Beijing, China, 3MR Application Predevelopment, Siemens Healthcare, Erlangen, Germany
Synopsis
This study aimed to investigate the utility of intra-voxel incoherent motion diffusion-weighted imaging (IVIM-DWI) for monitoring the liver function change during type 2 diabetes mellitus (T2DM) treatment. The results showed that liver fat fractions were significantly decreased and perfusion-related diffusion (D*) was significantly increased, but pure molecular diffusion (D) values showed no significant change in T2DM patients after treatment for three months. Our findings indicated that improvement of hepatic parenchymal perfusion may occur earlier than water molecule diffusion during T2DM treatment. D* may be a more sensitive biomarker than D to characterize the liver function change during T2DM treatment.
Introduction:
Nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus (T2DM) frequently coexist as they share the pathogenic abnormalities of excess adiposity and insulin resistance, which makes T2DM an excellent model of choice for investigating liver steatosis. Recent studies found that liver fat content could strongly affect the liver diffusion-weighted imaging (DWI) parameters such as perfusion fraction (f), pure molecular diffusion (D), perfusion-related diffusion (D*), and the apparent diffusion coefficient (ADC). For the fatty liver group, significantly lower ADC, D, and D* but significantly higher f have been reported than for the normal control group [1, 2]. These findings may provide more indicators to evaluate the liver function in T2DM with NAFLD. However, the efficacy of these parameters to monitor the liver function change during T2DM treatment remains unknown. Thus, this study investigated the change of liver IVIM-DWI parameters in T2DM patients before and after treatment, as well as its association with alterations in the liver fat fractions (LFCs).Materials and Methods:
This prospective study identified 26 T2DM patients (18 males; mean age, 48 years, range, 32 to 65 years). Patients received Acarbose (150 mg/d) and a lifestyle intervention (including diet control and exercise) for three months. Livers underwent pre- and post-treatment MR imaging on a 1.5T scanner (MAGNETOM Sempra, Siemens Shenzhen Magnetic Resonance Ltd., Shenzhen, China) equipped with a 6-channel body coil. Single-voxel MR spectroscopic data were used to calculate LFCs using a high-speed T2-corrected multi-echo (HISTO) sequence (TR = 3000 ms; 5 TEs = 15, 24, 36, 48, and 72 ms; and acquisition time = 15 s) with a 3x3x3 mm3 (27 mL) voxel positioned on segment VII. IVIM-DWI was performed using an echo-planar imaging sequence with 8 b-values (0, 50, 100, 150, 200, 300, 500, and 800 sec/mm2).The LFCs were automatically calculated. Hepatic steatosis was defined as having an LFC of at least 5.56%. The ADC and IVIM parameters including f, D, and D* were generated with the syngo.via Frontier MR Body Diffusion Toolbox prototype (Siemens Healthcare, Erlangen, Germany). Two radiologists blinded to clinical information analyzed the data independently. Paired t-tests were used to find differences in LFCs, ADC, FPs, D, and D* pre- and post-treatment. Significance was set at a P < 0.05.
Results:
Seventeen of twenty-six patients had liver steatosis at baseline. The liver fat data and quantitative DWI parameters for one representative patient are shown in Figures 1 and 2, respectively.Compared with the baseline values, LFCs (11.11% ± 6.87 vs. 8.91% ± 4.98, P = 0.002) were significantly decreased after treatment. The ADC (1.19 ± 0.11 x 10-3 mm2/s vs. 1.23 ± 0.10 x 10-3 mm2/s,P = 0.022) and IVIM parameters including D* (152.3± 35.8 x 10-3 mm2/s vs. 180.2 ± 40.5 × 10-3 mm2/s, P = 0.001) and (0.32 ± 0.08 vs. 0.34 ± 0.08, P = 0.019) were significantly increased after treatment. No significant differences were found in the D values between pre- and post-treatment (0.88 ± 0.19 × 10-3 mm2/s vs. 0.94 ± 0.21 × 10-3 mm2/s, P = 0.069).
Discussion:
Our results showed that the LFCs in T2DM patients were significantly reduced after therapy, suggesting that a lifestyle intervention could effectively reduce the liver fat deposition by regulating the metabolism of energy substances.Previous studies found that D* was significantly reduced in cases of steatosis and attributed this to the notion that enlargement of steatotic hepatocytes may narrow and deform the lumen of sinusoids, thereby decreasing hepatic parenchymal perfusion [3]. Some studies also found lower D or ADC values in the fatty liver and explained that the increased fat content of liver cells and extracellular fat accumulation reduced the interstitial space and restricted water diffusion, thereby resulting in a lower D or ADC. Interestingly, this study found that the IVIM parameters perfusion-related diffusion (D*) and perfusion-fraction (f) were significantly increased, but pure molecular diffusion (D) values had no significant change post-treatment. Our findings indicated that the improvement of hepatic parenchymal perfusion may be earlier than water molecular diffusion during T2DM treatment. Moreover, because the ADC calculation involved both pure molecular diffusion and capillary perfusion; the increased ADC in this study may be caused by increased microcirculation in the liver.
Conclusion:
D* may be a more sensitive biomarker than D and ADC to characterize the liver function change during T2DM treatment.Acknowledgements
This research was supported by the National Key R&D Program of China (2017YFE0103600), National Natural Science Foundation of China (81720108021, 81601466), and Zhongyuan Thousand Talents Plan Project-- Basic Research Leader Talent (ZYQR201810117).References
[1] Guiu B, Petit JM, Capitan V, et al. Intravoxel incoherent motion diffusion-weighted imaging in nonalcoholic fatty liver disease: a 3.0-T MR study. Radiology. 2012. 265(1): 96-103.
[2] Poyraz AK, Onur MR, Kocakoç E, Oğur E. Diffusion-weighted MRI of fatty liver. J Magn Reson Imaging. 2012. 35(5): 1108-11.
[3] McCuskey RS, Ito Y, Robertson GR, McCuskey MK, Perry M, Farrell GC. Hepatic microvascular dysfunction during evolution of dietary steatohepatitis in mice. Hepatology. 2004. 40(2): 386-93.
Figures
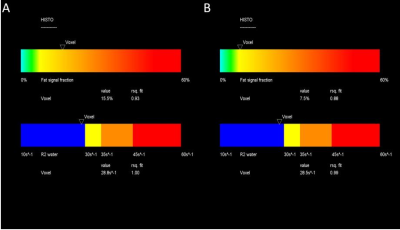
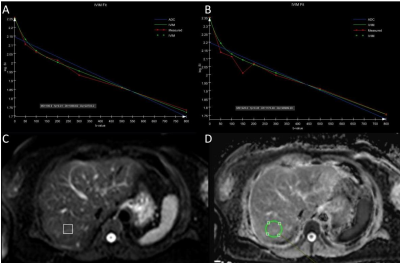
Figure 2. IVIM data for the same patient before (A) and after (B) treatment. IVIM parameters were calculated using a pixel lens which was positioned on segment VII (C). The results showed that fp, Dt, and Dp increased from 0.31 to 0.35, 1.07 × 10-3 to 1.18 × 10-3 mm2/s, and 227 × 10-3 to 290 × 10-3mm2/s, respectively. Dt (µm2/s) represents molecular diffusion and Dp (µm2/s) represents perfusion-related diffusion.The ADC value was calculated by placing an ROI at the same position (D). The results showed that ADC increased from 1.26 x 10-3 to 1.33 x 10-3 mm2/s. (Note: Dt = D, Dp = D*, and fp = f).