2621
Flow quantification with navigator-gated 4D flow MRI in portal hypertension1BioMedical Engineering and Imaging Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 2Department of Diagnostic, Molecular and Interventional Radiology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 3Department of Radiology, Weill Cornell Medicine, New York, NY, United States, 4Department of Radiology, Northwestern University, Chicago, IL, United States, 5Department of Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 6Department of Pathology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 7Biomedical Engineering, Northwestern University McCormick School of Engineering, Evanston, IL, United States
Synopsis
The purpose of our prospective study was to correlate the hepatic vasculature hemodynamic parameters measured with navigator-gated 4D flow MRI with the hepatic venous pressure gradient (HVPG) in patients with chronic liver disease and suspicion of portal hypertension (PH). Peak velocity in the celiac trunk (CT) was moderately correlated with HVPG, and was significantly elevated in patients with PH. CT flow was significantly elevated in patients with clinically significant PH (CSPH), while portal vein peak velocity was significantly reduced in patients with cirrhosis. Our results suggest that 4D flow MRI may be sensitive to hemodynamic changes in patients with PH.
Introduction
4D flow MRI has shown promise in the characterization of portal hypertension, however, clinical adoption has been slow due to long acquisition times and complex processing. The purpose of our study was to correlate the hepatic vasculature hemodynamic parameters measured with navigator-gated 4D flow with the hepatic venous pressure gradient (HVPG) in patients with chronic liver disease and suspicion of portal hypertension (PH).Materials and Methods
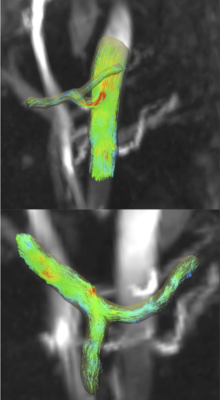
Twenty initial patients (M/F 12/8, mean age 56 y) with chronic liver disease and suspicion of portal hypertension were enrolled in our prospective study. Seventeen of 20 patients had transjugular liver biopsy with HVPG measurements (8.5± 5.8 mmHg, 0-18mmHg) within one month of multiparametric abdominal MRI at 1.5T on a clinical system (Aera, Siemens Healthcare, Erlangen, Germany). Phase-contrast MRI data was acquired 10 min. after injection of gadoxetic acid with a prototype respiratory navigator-gated 4D flow MRI sequence using RespiratoryControlled Adaptive k-space Reordering (ReCAR)1 technology. The acquisition covered the abdominal vessels in coronal-oblique orientation (VENC of 60 cm/sec, TR/TE/FA: 5.9 ms/3.4 ms/15°, 3 k-space segments/cardiac frame, 70.8 ms temporal resolution, 9-12 cardiac phases, 24 slices, resolution 2.5x2.5x2.5mm3). The portal (PV), superior mesenteric (SMV), splenic (SV) and middle hepatic veins (MHV), the supraceliac aorta and its celiac branches were segmented (Fig.1) using a centerline detection algorithm2 in prototype software (Siemens Healthcare, Erlangen, Germany). A single cross-sectional plane perpendicular to each vessel, placed in areas of high streamline density, was used for measurements. Two independent observers performed vessel segmentations, and measured time-averaged vessel cross-section area, through-plane time-averaged and peak velocity and flow. Interobserver agreement in vessel identification was determined by Cohen’s kappa, while interobserver agreement of measurements was evaluated by coefficient of variation (CV) and Bland-Altman statistics. Hemodynamic parameters were compared between patient groups according to PH and cirrhosis status by Mann-Whitney tests, and correlated with HVPG using Spearman correlations.Results
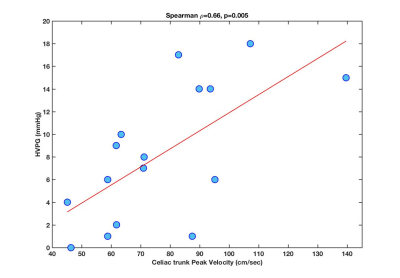
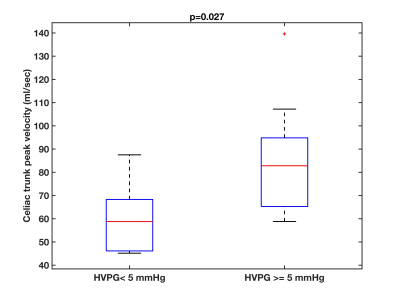
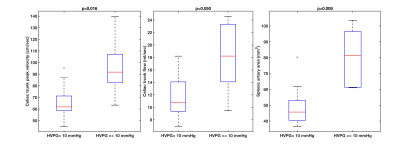
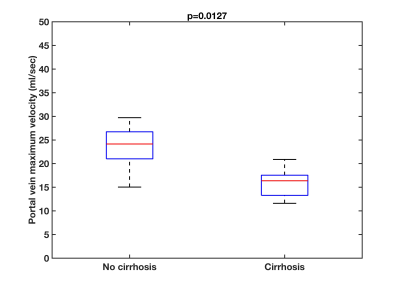
Acquisition time for the 4D flow MRI sequence was 9:17 min±1:41 min. Vessels were identified with substantial interobserver agreement (Cohen’s kappa=0.88, p<0.001). There was moderate interobserver agreement of hemodynamic measurements (CV<20%, Bland-Altman bias<20%, limits of agreement(%)=[-90,90]), which improved to good interobserver agreement for large vessels (PV, supraceliac aorta; CV<10%, Bland-Altman bias<5%, limits of agreement (%)=[-45,45]). Peak velocity in the celiac trunk (CT) positively correlated with HVPG (Fig. 2; Spearman r=0.66, p=0.005). CT peak velocity was significantly elevated (Fig. 3; p=0.027) in patients with PH (HVPG≥5mmHg) compared to those without. CT peak velocity (p=0.016), flow (p=0.05), and splenic artery area (p=0.008) were significantly elevated (Fig. 4) in patients with clinically significant PH (CSPH; HVPG≥10 mmHg) compared to those with no PH or PH (HVPG<10mmHg). PV peak velocity was significantly reduced (p=0.0127) in 8 patients with cirrhosis compared to 9 patients without cirrhosis (Fig. 5).Discussion
Blood flow measurements in abdominal vessels with the navigator-gated 4D flow MRI sequence have shown acceptable interobserver reproducibility. Interobserver reproducibility for vessel identification was comparable to reported values in the portal circulation using a Cartesian 4D flow respiratory gated acquisition with 20 min. acquisition time3. The reduction in PV velocity with cirrhosis confirms similar findings4-6. The correlation of celiac trunk velocity with HVPG and the elevated hemodynamic parameters in patients with PH are consistent with hyperdynamic arterial circulation in portal hypertension6. Future work will focus on validation of semi-automatic analysis tools7 that would provide hemodynamic measurements in multiple cross-sectional planes along the entire segmented length of abdominal vessels.Conclusion
4D flow MRI is sensitive to hemodynamic changes in patients with portal hypertension. The correlation with the degree of portal hypertension will be validated in a larger patient cohort.Acknowledgements
This research was supported by NIDDK grant 1R01DK113272. Many thanks to Ning Jin, PhD, and Andreas Greiser, PhD (Siemens Healthcare), developers of the 4D flow prototype sequence with ReCAR navigator, for disseminating and supporting the prototype sequence at our institution for research in liver MRI.References
1. Jin N, Greiser A, Chow K, et al. Respiratory Controlled Adaptive K-space Reordering (ReCAR) Improves 4D Flow Image Quality. In: ISMRM Honolulu, Hawaii, 2017
2. Gulsun MA, Jolly M-P, Guehring J, et al. A Novel 4D Flow Tool for Comprehensive Blood Flow Analysis. In: ISMRM, Melbourne, Australia, 2012
3. Stankovic Z, Frydrychowicz A, Csatari Z, et al. MR-based visualization and quantification of three-dimensional flow characteristics in the portal venous system. Journal of magnetic resonance imaging : JMRI 2010;32(2):466-475.
4. Stankovic Z, Csatari Z, Deibert P, et al. A feasibility study to evaluate splanchnic arterial and venous hemodynamics by flow-sensitive 4D MRI compared with Doppler ultrasound in patients with cirrhosis and controls. European journal of gastroenterology & hepatology 2013;25(6):669-675
5. Gouya H, Grabar S, Vignaux O, et al. Portal hypertension in patients with cirrhosis: indirect assessment of hepatic venous pressure gradient by measuring azygos flow with 2D-cine phase-contrast magnetic resonance imaging. European radiology 2016;26(7):1981-1990.
6. Roldan-Alzate A, Frydrychowicz A, Niespodzany E, et al. In vivo validation of 4D flow MRI for assessing the hemodynamics of portal hypertension. Journal of magnetic resonance imaging : JMRI 2013;37(5):1100-1108.
7. Vali A, Aristova M, Vakil P, et al. Semi-automated analysis of 4D flow MRI to assess the hemodynamic impact of intracranial atherosclerotic disease. Magnetic resonance in medicine 2019;82(2):749-762.
Figures