2603
Deep learning based image reconstruction for T2-weighted rectal cancer imaging1Department of Imaging Physics, The University of Texas M.D. Anderson Cancer Center, Houston, TX, United States, 2MR Applications and Workflow, GE Healthcare, Waukesha, WI, United States, 3Department of Radiology, The University of Texas M.D. Anderson Cancer Center, Houston, TX, United States, 4Department of Surgical Oncology, The University of Texas M.D. Anderson Cancer Center, Houston, TX, United States, 5Department of Pathology, The University of Texas M.D. Anderson Cancer Center, Houston, TX, United States
Synopsis
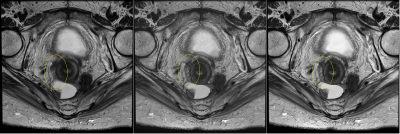
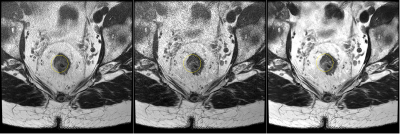
Proper evaluation of rectal cancer with MR imaging requires high resolution imaging of the rectal wall. The image quality demands are difficult to achieve due to the increasing risk of peristaltic motion with longer scan times. In this work, we apply a novel deep learning based reconstruction (DL recon) method to an accelerated sequence using reduced averages and increased acceleration. Radiologist scores indicate that the combined method provides superior SNR and definition with less motion degradation when compared to the routine sequence with conventional reconstruction. Thus improved motion robustness can be gained from applying DL Recon to an accelerated sequence.
Introduction
MRI is the modality of choice and standard of care for rectal cancer imaging because it provides excellent visualization of the tumor relative to the rectal wall, mesorectum, and surrounding structures. Among the different sequences used, high quality and high-resolution T2-weighted imaging is the most important component of a rectal cancer MRI protocol [1]. Because of the resolution and SNR requirement, multiple signal averages and long scan time (often greater than 5 minutes per series) are often used, which in turn renders the sequence susceptible to motion (such as from the peristalsis) and the images blurred. Deep learning based image reconstruction (DL Recon) offers the potential for substantially reduced scan time without an apparent penalty to SNR, and thus reduced susceptibility to motion. In this work, we investigate using a novel DL Recon for high resolution T2-weighted rectal cancer imaging at accelerated acquisition speed.Methods
The DL Recon used in our study is a deep convolutional residual encoder network trained to reconstruct images from 2D MR data with reduced noise, reduced Gibbs ringing, and enhanced resolution. The network has an adjustable parameter that ranges between 0 and 100% to control the noise level of the final reconstructed images.Fifteen patients were included in this study to evaluate DL Recon in comparison to conventional reconstruction on a high resolution oblique axial T2-weighted sequence in our standard rectal protocol. The subjects were scanned on several different 3T clinical scanners (MR750w and Signa PETMR, GE Healthcare, Waueksha, WI). The slices in this sequence were positioned axially through the rectum covering the entire tumor. The routine protocol scan parameters for the sequence were matrix = 320x256, FOV = 20cm, thickness/gap = 3mm / 1mm, ETL=24, bandwidth = ±41.67kHz, TR>6000msec (adjusted to fit number of slices), ARC acceleration factor = 1.5, NEX=4. Total scan time was typically 5 minutes for 30 slices. The same scan coverage and scan parameters were repeated in a separate series for DL Recon, except NEX was reduced to 2 and ARC acceleration factor was increased to 2.0, reducing overall scan time to just over 2 minutes for 30 slices. The data from the shorter acquisition were reconstructed using both DL Recon (at 75% noise level reduction) and the conventional reconstruction.
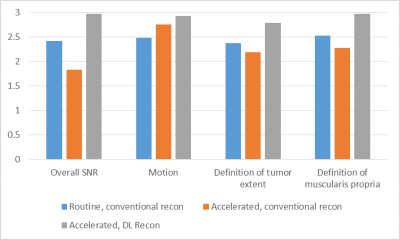
Three radiologists rated the three sets of images: the standard sequence with conventional reconstruction, the accelerated sequence with conventional reconstruction, and the accelerated sequence with DL Recon. Images were qualitatively scored on a 3-point Likert scale for the following categories: overall SNR, severity of motion degradation, definition of tumor extent, and definition of the muscularis propria.
Results
Radiologist scores are shown in Figure 1. Overall, the accelerated sequence reconstructed with DL Recon scored higher than both the routine and accelerated sequence with conventional reconstruction across all categories: overall SNR (2.98 vs. 2.41 and 1.83), motion (2.93 vs 2.49 and 2.76), definition of tumor extent (2.78 vs 2.38 and 2.19), and definition of muscularis propria (2.97 vs 2.53 and 2.28). With conventional reconstruction, the accelerated sequence scored the worst for overall SNR, definition of tumor extent, and definition of the muscularis propria. The routine scan parameters with conventional reconstruction scored the worst for severity of motion degradation.Discussion
Compared to our standard acquisition with conventional reconstruction, DL Recon applied to an accelerated acquisition produced higher diagnostic quality images in less than half the scan time, with less image degradation from motion. SNR, resolution, contrast, and lack of motion related artifacts or blurring are all important for visualization of the thin submucosa and muscularis propria layers of the rectal wall. Since staging of the tumor is dependent on which layer the tumor has invaded [2,3], achieving consistent image quality is critical to properly diagnosing the tumor and making appropriate treatment decisions.As an image enhancement technique, DL Recon would expected to improve measures of SNR and resolution. Our study shows that it does not affect other image quality metrics such as shading or presence of flow artifacts. Since it was not designed to correct for motion degradation, the motion related benefits come from reducing overall motion during the reduced acquisition time. Even when the patient is voluntarily able to remain motionless during the entire sequence, the rectum may still involuntarily move due to peristalsis. We therefore conclude that DL recon can be advantageously applied to improve image quality while reducing overall scan time, which synergistically also reduces risk of sporadic motion or the severity of blurring from slow, continuous motion.
Image filtering techniques have been known to affect resolution while some iterative denoising methods could remove fine structures or affect the overall “look” of the images. By working with complex raw data, DL Recon is able to tolerate a higher noise level before exhibiting such effects, which were not observed in our study.
In conclusion, DL Recon was shown to substantially reduce the total scan time for high resolution T2-weighted imaging of rectal cancer, with improvement in SNR and visualization of structures for the evaluation of rectal cancer, while noticeably reducing the motion artefacts when compared to the standard protocol.
Acknowledgements
Prototype DL Recon and support was provided by GE Healthcare.References
1. Gollub MJ, et al. Use of magnetic resonance imaging in rectal cancer patients: Society of Abdominal Radiology (SAR) rectal cancer disease-focused panel (DFP) recommendations 2017. Abdom Radiol. 2018;43:2893-2902.
2. Horvat N, et al. MRI of Rectal Cancer: Tumor Staging, Imaging Techniques, and Management. Radiographics. 2019;39:367-387.
3. Glynne-Jones R, et al; ESMO Guidelines Committee. Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(suppl_4):iv22-iv40.
Figures