2584
Levator hiatus width measurement and its correlation with pelvic floor dysfunction1Body MRI, Stanford University, PALO ALTO, CA, United States, 2Mathematics, Oakland University, Rochester, MI, United States
Synopsis
Pelvic floor dysfunction affects about half of women over 50 years of age, causing significant morbidity. MR defecography compliments the clinical examination in the evaluation of pelvic floor dysfunction. We investigated if the measurement of levator hiatus width is a useful and reliable supplement or alternative measurement in predicting pelvic floor dysfunction. We retrospectively reviewed MR defecography examinations and recalculated the levator hiatus width and the anorectal angle with 2 blinded readers. We found that the levator hiatus width had a statistically significant correlation with pelvic organ prolapse and can add to the confidence in reporting H-line and M-line abnormalities.
Synopsis:
Pelvic floor dysfunction affects about half of women over the age of 50 years and causes significant morbidity. MR defecography compliments the clinical examination which was once the primary method of evaluating pelvic floor dysfunction. We investigated if the measurement of levator hiatus width is a useful and reliable supplement or alternative measurement in predicting pelvic floor dysfunction. We retrospectively reviewed MR defecography examinations and recalculated the levator hiatus width and the anorectal angle with 2 blinded readers. We found that the levator hiatus width had a statistically significant correlation with pelvic organ prolapse and can add to the confidence in reporting H-line and M-line abnormalities.Introduction
Interpretation of MR defecography examinations for evaluating pelvic floor dysfunction traditionally includes assessment of H- and M-line measurements along with anorectal angle measurements. Especially with real-time imaging of Kegel and defecation maneuvers, MR defecography is more widely used than the conventional fluoroscopic defecography. Abnormal H-line and M-line measurements reflect the increased diameter of the levator hiatus and pelvic floor descent. Assessment of the puborectalis muscle which is one of the three important components of the levator ani muscle complex which supports the pelvic floor is usually qualitative. Levator hiatus width (LHW) and puborectalis thickness (PT) are additional simple adjunct measurements that have been proposed in the literature, but the value of these measurements has not been well established. The objective of our study was to correlate LHW measurement to the H-line and M-line to the presence of pelvic organ prolapse and evaluate the reliability of these measurements between readers.Methods
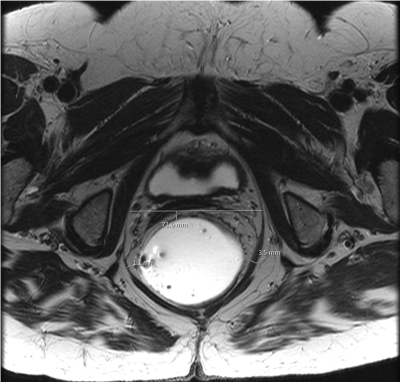
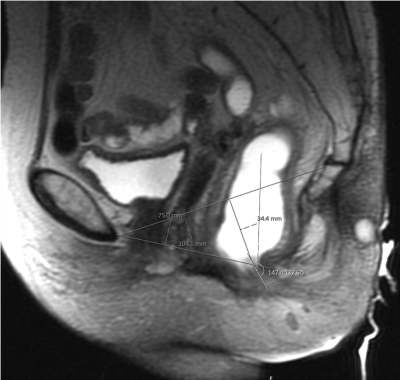
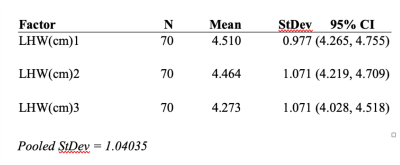
A retrospective review of 70 consecutive MR defecography examinations in female patients performed on 3T MRI scanners in a single institution over a period of 4 months (May 2019- August 2019) was analyzed. As part of the MR defecography examination, axial T2 weighted images of the pelvis were obtained as axial to body plane (4 mm slice thickness, TR 800, TE 150, FOV 24 cm, 512 x 256 matrix). Based on the literature review, the LHW measurement of 4.5 cm was selected as normal cut off measurement which is measured at the inferior margin of the pubic symphysis, between the medial margins of the puborectalis muscle in the resting phase of the examination protocol [Figure 1]. PT was measured at the same level for the thickness of the muscle, and asymmetric muscle thickness was documented. The images were reviewed, and the following was documented for analysis: age of the patient, LHW, PT, H-line, M-line, anorectal angle (ARA) measurements in resting, during Kegel maneuver and dynamic defecation. Based on the measurements, the anterior, middle and posterior compartment pelvic floor descent was graded and compared with LHW and PT measurements. Reader 1 in our analysis was the board-certified radiologist who had initially reported the examination (this represented a pool of body radiologists as well as body radiologist specialized in reading MRI), Reader 2 is a board-eligible body MRI fellow, and reader 3 is a board-certified radiologist with expertise in reporting MR defecography. The second and third readers were blinded to the clinical details and radiology report. The reader 2 and 3 re-measured the LHW and PT, and reader 3 also re-measured the anorectal angles, H-line, and M-line of the study patients.One-way ANOVA, Tukey pairwise comparisons, Fischer’s exact test, chi-square test, and descriptive statistics for interobserver variability were used for statistical analysis.
Results
The mean age of our study population was 59 years. The mean LHW was 4.2 cm to 4.5 cm among the three readers. The percent of abnormal LHW classifications for the readers 1,2, and 3 are 39%, 34%, and 29% respectively. Reader 3 has the lowest tendency for abnormal measurement of LHW. We found that the mean puborectalis muscle thickness was 5.1 mm (right- 5.13 mm and left- 5.07 mm), of which 68.57% has symmetric puborectalis muscle and 31.43% of patients had asymmetric muscle thickness. Using Fischer’s exact test, there was a statistically significant correlation between the defecation H-line with the bladder descent (p=0.001), and uterine descent (p=0.004), vaginal descent (p=0.02), anterior rectocele (p=0.03). Overall, the descent of any pelvic organ and defecation H-line was statistically significant with p=0.0001.Based on Fisher’s exact method, there was no statistically significant difference between the subspeciality of the readers in interpreting the levator hiatus width (p=0.220). There was 81.43% agreement between the readers 1 and 3, and 91.43% agreement between readers 2 and 3.
Discussion
Levator hiatus width measurement can be used to complement the H-line and M-line measurements at rest to help in the diagnosis of pelvic organ prolapse. We found that variations in the LHW measurements among the readers were greater between readers with and without specific expertise in the interpretation of MR defecography. Training can reduce interobserver variability in interpretations.Conclusion
LHW measurement has a statistically significant correlation with pelvic floor relaxation and descent, hence it can be used in conjunction with H- and M-lines to determine pelvic floor dysfunction for added confidence. This has not previously been reported in the literature. We also propose that puborectalis thickness <5 mm, especially in the presence of asymmetric thinning or defect can help in the evaluation of pelvic descent.Acknowledgements
No acknowledgement found.References
1. Dietz HP, Severino M, Atan IK, Shek KL, Rojas RG. Warping of the levator hiatus: how significant is it? Ultrasound Obstet Gynecol 2016;48:239-242.
2. Gregory WT, Nardos R, Worstell T, Thurmond A. Measuring the levator hiatus with axial MRI sequences: Adjusting the angle of acquisition. Neurourology and Urodynamics 2011;30:113-116.
3. Cholaiacomo MC, Masselli G, Polettini E, Lanciotti S, Casciani E, Bertini L, Gualdi G. Dynamic MR Imaging of the pelvic floor: a pictorial review. Radiographics 2009;29:3,e35.
4. de Salto LG, Criado JM, Velasco lG, et al. MR Imaging-based assessment of the female pelvic floor. Radiographics 2014;34:1417-1439.
Figures