2579
MRI Changes in Visceral Fat in Crohn’s Disease1Sir Peter Mansfield Imaging Centre, School of Physics, University of Nottingham, Nottingham, United Kingdom, 2Nottingham Digestive Disease Biomedical Research Centre, University of Nottingham, Nottingham, United Kingdom, 3Metabolic and Molecular Physiology, School of Life Sciences, University of Nottingham, Queen's Medical Centre Campus, Nottingham, United Kingdom
Synopsis
Crohn’s disease (CD) is an inflammatory bowel disease which effects 150k people in the UK alone. Visceral fat hypertrophy is a characteristic radiological finding in CD.To date radiologists just describe it but are not able to provide more objective data regarding visceral fat volume. In this retrospective study we used 2-point mDixon fat Images along with image processing techniques to study visceral fat properties in CD patients compared with healthy volunteers. The data demonstrated a tendency of CD patients to have a higher ratio of visceral fat and more volume of intestines fully surrounded by fat compared with healthy volunteers.
Introduction
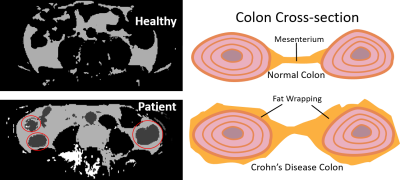
Crohn’s disease (CD) is a chronic, relapsing and remitting inflammatory disease of the gastrointestinal (GI) tract affecting 150k people in the UK [1]. The traditional management of CD involves a stepwise escalation of treatment. However, this approach can lead to a delay in those at high risk of disease progression. The correlation between symptoms and endoscopic disease activity is poor so there is a risk of under treatment [2]. Objective evidence of inflammation is required when considering treatment alterations. Hence, inflammation resolution on cross sectional imaging is suggested as an alternative to invasive endoscopy [3]. Fat wrapping refers to the hypertrophy of mesenteric fat to partially cover the small or large intestine. In CD, adipose tissue accumulation is localized around the inflamed intestinal segments. As a result, CD patients tend to have higher ratio of intra-abdominal visceral fat (VAT) to total abdominal fat when compared with healthy controls [4, 5]. Although visceral fat hypertrophy is subjectively commented upon by radiologists, no automated quantitative measures were developed to adequately evaluate the effects of fat wrapping in CD.Aim : To Investigate the effects of fat wrapping in CD by measuring abdominal VAT volume and distribution in CD patients compared to healthy controls.
Methods
We developed an automated segmentation software in MATLAB (Mathsworks, Natick, MA, USA) to segment fat only images derived from 2 point mDixon MRI data (acquired on Philips 1.5 T and 3.0 T MRI scanners) into visceral (VAT) and Subcutaneous (SAT) adipose tissue. The algorithm relies on analyzing the abdominal fat shapes and estimating the intra-abdominal using a combination of filters and morphological processes. In order to validate the resulting segmentation (Fig 1), the segmentations were compared to manually segmented images on each slice axial slice using the Sørensen–Dice coefficient [6]. Seven data sets were used for this validation. To study the effect of fat wrapping in CD a retrospective study was then performed on 19 healthy volunteers (6 Females and 13 Males) with BMI = 26±5 kg/m2 and 17 CD patients (8 Females and 9 Males) with BMI = 25±3 kg/m2 scanned using mDixon across the abdominal area between L3-S1. The algorithm was used to calculate the ratio of VAT to total abdominal fat volume. Next it was used to determine the ratio of the volume of the intestines that were fully surrounded by fat to total volume of intestines, by automatically searching for holes in the visceral fat regions which are large enough to be filled by intestines as shown inFigure 2. Finally the inter-abdominal area was also segmented into right side and left side by automatically drawing a line along the spine and the ratios of fat one the right side over total abdominal fat volume was calculated.
Results
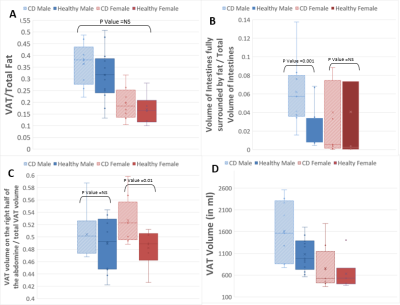
The segmentation algorithm performance gave Dice coefficients of 0.95±0.016 for automatic compared to manual VAT segmentation and 0.98±0.005 for SAT segmentation. Figure 3A shows the ratio of VAT to total abdominal fat volume was slightly greater in CD than healthy controls but with non-significant P-Value. Figure 3B shows the ratio of intestinal volume fully surrounded by fat to the total volume of intestines is greater in male patients with CD (p=0.01).Figure 3C shows the ratio of fat on the right side of the abdomen to total visceral fat was significantly higher for CD patients than healthy controls (p=0.17) overall but dominated by female subjects. Figure 3D shows absolute VAT volumes in CD and healthy volunteers for comparison.
Discussion
The retrospective study data demonstrated a trend for CD patients to have a slightly higher ratio of VAT to total abdominal fat and more volume of intestines fully surrounded by fat when compared with healthy controls, although this affects males more than the females. Figure 4 shows that CD patients tend to have a higher VAT fat ratio on the right side of the abdomen when compared with healthy control which correspond to the ascending colon and terminal ileum where the greatest fat wrapping for ileal crohn's disease would be expected, but this affects females more than males. We have split the data by sex as gender differences are expected in abdominal fat distributions, but it is important to point out that by separating male and female data, the sample size is reduced and therefore anomalous results affect these group level results. This work needs to be extended to larger groups of patients with a wider range of BMI, and with retrospective surgical confirmation of the results.Conclusion
These potential new markers of fat wrapping may provide clinically useful, relatively simple additional new markers of inflammation in crohn’s disease.Acknowledgements
This work is funded by the Biomedical Research center and The Haydn Green institute for innovation and entrepreneurship.References
[1] Mayberry, J. F., Lobo, A., Ford, A. C., & Thomas, A. (2013). NICE clinical guideline (CG152): The management of Crohn’s disease in adults, children and young people. Alimentary Pharmacology and Therapeutics.
[2] Gracie, D. J., Williams, C. J. M., Sood, R., Mumtaz, S., Bholah, M. H., Hamlin, P. J., & Ford, A. C. (2016). Poor correlation between clinical disease activity and mucosal inflammation, and the role of psychological comorbidity, in inflammatory bowel disease.
[3] Miles, A., Bhatnagar, G., Halligan, S., Gupta, A., Tolan, D., Zealley, I., … Duncan, G. (2019). Magnetic resonance enterography, small bowel ultrasound and colonoscopy to diagnose and stage Crohn’s disease: patient acceptability and perceived burden.
[4] Lancet Gastroenterology and Hepatology. Thiberge, C., Charpentier, C., Gillibert, A., Modzelewski, R., Dacher, J. N., Savoye, G., & Savoye-Collet, C. (2018). Lower subcutaneous or visceral adiposity assessed by abdominal computed tomography could predict adverse outcome in patients with Crohn’s disease. Journal of Crohn’s and Colitis, 12(12), 1429–1437.
[5] Cravo, M. L., Velho, S., Torres, J., Costa Santos, M. P., Palmela, C., Cruz, R., … Baracos, V. (2017). Lower skeletal muscle attenuation and high visceral fat index are associated with complicated disease in patients with Crohn’s disease: An exploratory study. Clinical Nutrition ESPEN, 21, 79–85.
[6] Zou, K. H., Warfield, S. K., Bharatha, A., Tempany, C. M. C., Kaus, M. R., Haker, S. J., … Kikinis, R. (2004). Statistical Validation of Image Segmentation Quality Based on a Spatial Overlap Index. Academic Radiology.
Figures
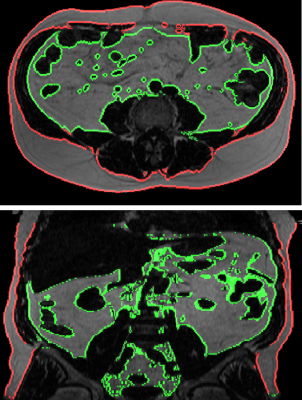
Figure 1. Segmentation of visceral fat (red) and subcutaneous fat (green) using the developed automated method. Top image – axial slice, bottom image reformatted coronal slice.