2571
Upright pelvimetry using MRI for the prediction of birth associated cephalo-pelvic disproportion following induction of labour.1Sir Peter Mansfield Imaging Centre, University of Nottingham, Nottingham, United Kingdom, 2Queens Medical Centre, NUH NHS Trust, Nottingham, United Kingdom, 3Faculty of Medicine and Health, University of Nottingham, Nottingham, United Kingdom
Synopsis
Dystocia, difficult birth due to either a big baby, small maternal pelvis, or malposition of the presenting part is an important obstetric problem and a major cause of emergency caesarean section and birth injury. The risk of caesarean section is 30% for first time mothers who have had their labour induced. We have developed an MRI protocol to assess fetal size and maternal pelvic measurements in supine and upright positions to determine whether they can be used as a predictor of a woman's risk of emergency C-section after the induction of labour.
Introduction
Dystocia, difficult birth due to either a big baby, small maternal pelvis, or malposition of the presenting part is an important obstetric problem and a major cause of emergency caesarean section and birth injury. The risk of caesarean section is 30% for first time mothers whose labour is induced. With better nutrition, the extremes of pelvic inadequacy (caused by malnutrition) are now rare and so imaging is required to identify subtle degrees of pelvic contraction. Previously this involved X-ray assessment, which was not informative, and carries some risk. Recent research has concentrated on identifying larger babies using ultrasound, which is operator dependent, not very accurate and unable to measure the maternal pelvis. Upright MRI has the potential to alter the whole picture. MRI has greater sensitivity than ultrasound for the detection of big babies (93% versus 56%) for estimated fetal weight above the 90th centile1), and can simultaneously provide detailed information on the conformation of the maternal pelvis which is essential to predict cephalo-pelvic disproportion and further relevant information on fetal anatomy (e.g. shoulder dimensions). Upright MRI allows the measurement of pelvic dimensions in supine, squatting or sitting positions which may alter the conformation of the pelvis in some women2.Aims:
1. To develop an MRI protocol to assess fetal size and maternal pelvic measurements in supine and upright positions as a predictor of a woman’s risk of emergency C-section after induction.
2.To measure fetal shoulder width and fetal volume with MRI.
3.To compare pelvic dimensions in the supine and upright positions for women in the late third trimester of pregnancy.
Methods
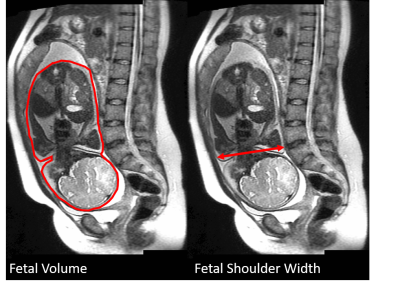
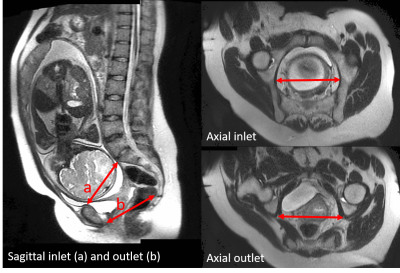
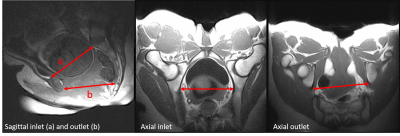
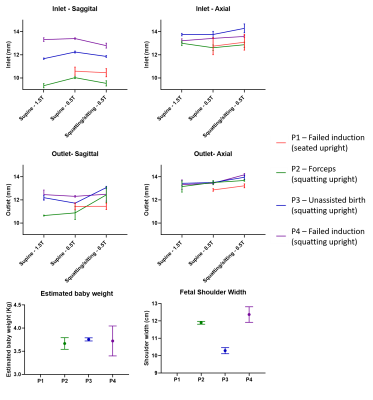
This study aims to recruit 50 women with local ethics approval. Currently 4 women with singleton pregnancies all who were due to be induced within a week of imaging have been recruited. The imaging protocol was split to require short scan sessions in two different scanners. The first was on a GE 1.5T MRI using a 12 channel body array coil (for foetal volume, shoulder measurements and maternal pelvimetry). The second was on a Paramed 0.5T Upright scanner using a flex spine coil for maternal pelvimetry measurements in various positions. Although fetal measurements are possible on the upright they were not made as they are not expected to change with maternal position. Fetal volume and shoulder width and maternal pelvimetry at 1.5T were measured from SSFSE acquisitions (resolution 0.93x0.93mm2, slice thickness 9mm, TE = 90ms and TR = 660ms, breath held), with the geometry adjusted to cover the whole foetus for the volume measurements and to give the fetal coronal cross section for the shoulder measurements. Upright pelvimetry measurements at 0.5T were made using a T1 weighted Spin Echo sequence (resolution 1.25x1.25mm2, slice thickness 6mm, TR=350ms and TE=12ms), acquired in two different positions, supine and sitting/squatting. Images were collected with sagittal and oblique axial slices to allow for pelvic inlet and pelvic outlet measurements to be made. All analysis was performed in MIPAV3. Fetal weight was estimated from the fetal volume (Figure 1) using Weight = 1.031(g/dm3) x fetal volume (dm3) +0.12(kg) 4. Shoulder measurements were calculated as the distance from the outer most part of the subcutaneous fat at the level of the shoulders (Figure 1). The pelvic inlet and outlet were measured on a sagittal slice and an axial oblique slice in both supine and sitting/squatting positions (Figures 2 and 3). The delivery method (vaginal birth (and notes of any assistance methods used) or emergency C-section) was recorded as well as the birth weight of the fetus.Results
The average MRI fetal weight was 3.6±0.1kg which correlated well with the birth weight (mean difference of 5%). The mean shoulder width was 11.6±1.9cm. The mean pelvic diameters (Figure 3) were 11.3±1.6cm and 11.9±0.6cm for the sagittal measures of inlet and outlet and 13.3±0.5cm and 13.4±0.3cm for the oblique axial measures of inlet and outlet. The delivery methods were vaginal birth with no assistance, vaginal birth with forceps, and emergency C-section due to failed induction of labour.Discussion
Whilst the numbers recruited for this study are currently small we have demonstrated that fetal and pelvimetry measurements can be made with MRI and upright MRI. We are currently exploring alternative methods of comfortably positioning a heavily pregnant woman in the upright scanner in one short visit. Numbers are currently too low for statistical evaluation but inlet and outlet pelvis measurements in the supine position seem consistent across both field strengths, whilst the squatting position showed differences when compared to the supine position. This suggests that changing position during birth could assist with opening the pelvis for some women. With larger numbers the relationship between squatting pelvic dimensions and supine pelvic dimensions will be investigated further as well as the relationship with birth outcomes and pelvic/fetal measurements.Conclusion
We have shown that MRI can be used to make both pelvimetry and fetal measurements in women who are having their labour induced in a short scanning session. We have also shown that upright MRI can be used to make pelvimetry measurements in both the supine and squatting positions.Acknowledgements
No acknowledgement found.References
1. G.L. Malin, G.J. Bugg, Y. Takwoingi, J.G. Thornton, N.W. Jones. Antenatal magnetic resonance imaging versus ultrasound for predicting neonatal macrosomia: a systematic review and meta-analysis. BJOG 2016;123:7
2. M. J. McAuliffe, F. M. Lalonde, D. McGarry, W. Gandler, K. Csaky, B. L Trus, "Medical image processing analysis and visualization in clinical research", 14 th IEEE CBMS Proceedings , pp. 381-386, 2001.
3. A. Hemmerich, T. Bandrowska, G. A. Dumas. The effects of squatting while pregnant on pelvic dimensions: A computational simulation to understand childbirth. Journal of Biomechanics p64-74, 2019
4. P.N. Baker, I.R. Johnson, P.A. Gowland, J. Hykin, PR. Harvey, A. Freeman, et al. Fetal weight estimation by echo-planar magnetic resonance imaging. Lancet. 1994;343(8898):644–5
Figures