2567
Imaging the Fetal Spine using MRI: A Preliminary Exploration on Scanning Strategy1radiology, Shandong Medical Imaging Research Institute, Shandong University, jinan, China, 2Shandong Medical Imaging Research Institute, Shandong University, jinan, China, 3MR Collaboration, Siemens Healthcare Ltd., beijing, China
Synopsis
This study explored the scanning strategy of fetal spine imaging using Magnetic Resonance Imaging (MRI) on 315 volunteer pregnant subjects. Whole-spine MRI was performed on fetuses using Susceptibility-Weighted Imaging (SWI) and True Fast Imaging with Steady-state Precession (TrueFISP) sequences. Images from both methods were acquired, and the diagnostic efficacy was compared. The SWI showed superior performance in visualizing osseous spinal anomalies, while TrueFISP better presented spinal canal contents lesions. Additionally, the MRI was preferred for the diagnosis of fetal spinal diseases to US. These mixed results suggest that a combination of both techniques is appropriate for fetal spine imaging.
Introduction
Imaging the spine’s anatomy and its relevant pathology is clinically important for the early identification of anomalous osseous development and lesions of spinal canal contents [1]. Previous studies of the assessment and recognition of the fetal osseous spinal anomalies or spinal canal contents lesions are found in the literature [2-3]. However, there is a lack of a systematic Magnetic Resonance Imaging (MRI) scan strategy. This study aimed to explore the diagnostic value of the MRI in the anatomical structure of fetal spine and related lesions, and to compare with ultrasonography (US).Materials and Methods
This retrospective study was approved by the local ethics review board and comprised 315 written-consenting pregnant women with suspected fetal spinal anomalies (screened by US) between Dec.2015 and Nov. 2019. All patients underwent US and MR examinations again at our tertiary-level institution. The MR examinations were performed on a 1.5T MAGNETOM Amira (Siemens, Shenzhen Magnetic Resonance Ltd., Shenzhen, China) with an 18-channel spine coil and a 13-channel body coil positioned over the lower pelvic area. The MR protocols included Susceptibility-Weighted Imaging (SWI) and True Fast Imaging with Steady-state Precession (TrueFISP). All images were obtained in axial, coronal, and sagittal planes. The fetal spine was classified into two groups according to the location of the lesion identified by the US as either, (a.) including osseous spinal anomalies (Group 1), or, (b.) spinal canal contents lesions (Group 2). Diagnosis of postnatal imaging was made via MR, computed tomography (CT), or X-Ray, and served as the reference standard for the final diagnosis in all cases. Then using Chi-square test analysis, the two groups were evaluated respectively with TrueFISP, SWI, and the combination of both. Sensitivity, specificity, and the accuracy rate between the sequence and the follow-up results were calculated. An estimate of degree of any improvements in diagnostic accuracy of MRI over US imaging was made by comparing the in-utero diagnoses performance with the final results made postnatally.Results
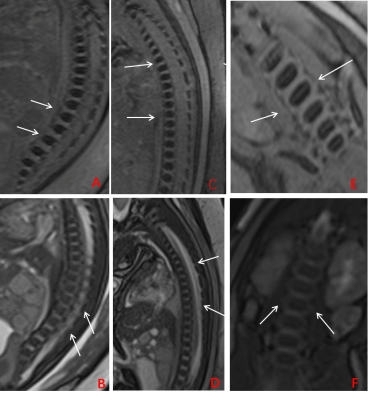
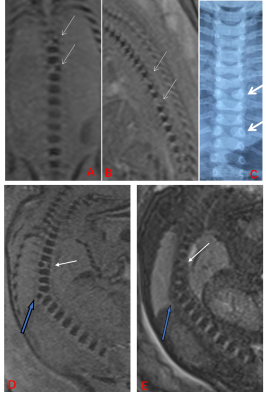
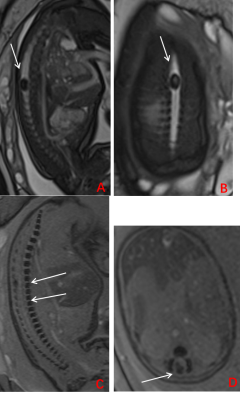
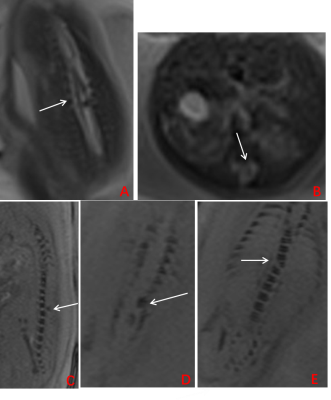
A total of 315 pregnant women were enrolled in the study (mean age, 30.3 ± 5.6 years, mean gestational age (GA), 29.3 ± 3.5 weekss, range GA 22~39 weeks), including fetuses with a normal spine (n=73, group 1, n=66; group 2, n=7 [Fig. 1]), osseous spinal anomalies (n= 141, [Fig. 2]) and spinal canal contents lesions (n=101, [Fig. 3, 4]). As a reference standard, 188 osseous spinal anomalies (n = 141) were identified on follow-up results including hemivertebrae (n = 64), butterfly vertebra (n = 43), block vertebrae (n = 53), coronal clefts (n = 22), and caudal regression syndrome (n = 6). The spinal canal contents lesions (n =101) consisted of spina bifida (n = 25), spinal canal content obtrusion (n=43), spinal canal neoplastic lesions (n =28), and diastematomyelia (n = 5). As shown in Table 1, SWI demonstrated higher diagnostic accuracy than TrueFISP for detecting osseous spinal anomalies (all P < 0.001). TrueFISP demonstrated higher diagnostic accuracy than SWI for detecting spinal canal contents lesions (P < 0.001 or 0.01). MRI was found to be significantly superior to US in the diagnosis of fetal spinal diseases (all P < 0.001).Discussion
Previous studies have identified that the scanning and detection of spinal malformations and lesions in utero remain a major challenge for radiologists and clinicians involved in antenatal diagnosis [4]. The results of this study demonstrated that SWI sequence could provide significantly higher diagnostic performance on fetal spine osseous developmental deformation. Likewise, the TrueFISP sequence showed superior performance for visualizing spinal canal contents lesions. TrueFISP combined with SWI sequence showed an overall improved diagnostic performance compared to that of any single sequence for the detection of probable osseous spinal anomalies and/or spinal canal contents lesions. This study also supports previous research that has shown that a relatively high proportion of diagnoses on US imaging are inaccurate [5]. Overall, the study’s findings suggest that a combination of both methods provides comprehensive results, an improvement over using either SWI or TrueFISP as a singular method, and may be a more practical strategy for clinicians to employ.Conclusion
A combined approach using TrueFISP with SWI sequence may provide greater value than the routine MRI scanning strategy to achieve the best diagnostic performance for fetal spinal osseous anomalies and relevant lesions in fetal spine imaging, particularly when a clear diagnosis cannot be achieved with US.Acknowledgements
The authors are grateful to Mrs. Chen for her valuable diagnostic assistance.References
- Garne, E., et al., Prenatal diagnosis of severe structural congenital malformations in Europe. Ultrasound in Obstetrics and Gynecology, 2005. 25(1): p. 6-11.
- Griffiths P D, Widjaja E, Paley M N J, et al. Imaging the fetal spine using in utero MR: diagnostic accuracy and impact on management[J]. Pediatric radiology, 2006, 36(9): 927-933.
- Robinson, A.J., et al., Foetal “black bone” MRI: utility in assessment of the foetal spine. The British Journal of Radiology, 2015. 88(1046): p. 20140496.
- Aaronson O S, Hernanz-Schulman M, Bruner J P, et al. Myelomeningocele: prenatal evaluation—comparison between transabdominal US and MR imaging[J]. Radiology, 2003, 227(3): 839-843.
- Griffiths P D,
Widjaja E, Paley M N J, et al. Imaging the fetal spine using in utero MR:
diagnostic accuracy and impact on management[J]. Pediatric radiology, 2006,
36(9): 927-933.
Figures
Table 1.
Note. —Data are number of lesions
Group 1= osseous spinal anomalies
Group 2= spinal canal contents lesions
a Statistical signifcance is denoted by p < 0.001
b Statistical signifcance is denoted by p < 0.01