2565
Comparison of ultrasound and magnetic resonance imaging for the detection of fetal corpus callosum abnormalities1Shandong Medical Imaging Research Institute, Shandong University, Jinan, China, 2MR Collaboration, Healthcare Siemens Ltd., Beijing, China, Beijing, China
Synopsis
We compared ultrasound and magnetic resonance imaging (MRI) for the detection of fetal corpus callosum (CC) dysplasia in 375 fetuses at our Institute. The results showed that MRI was significantly better than ultrasound in being able to diagnose normal and abnormal fetal CC. Also, fetal MRI can be helpful in assessing associated abnormalities and enhancing prognostic consultations.
Introduction
Agenesis of the corpus callosum (ACC) is one of the most common brain abnormalities diagnosed antenatally with an incidence of 0.05-0.7% in the general population and 2-3% in patients with mental deficiencies[1]. With the advantages of high resolution, large field of view, and lack of fetal position or amniotic fluid restrictions, MRI allows direct visualization to assess for the complete or partial absence of the CC. MRI can also help detect coexisting brain abnormalities not seen on ultrasound, such as gyration and heterotopia[2-3]. Although several studies have been conducted regarding the accuracy of ultrasound and MRI for the detection of fetal CC anomalies[4-7], no studies comparing the different types of fetal CC anomalies have been performed that include such a large number of patients as was used in the current study. In this study, we compared ultrasound and MRI for the detection of fetal CC dysplasia.Methods
This retrospective study was approved by our Institutional Review Board. All fetuses with suspected CC anomalies (screened by ultrasonography) and referred to or diagnosed at our institute between January 2014 and July 2019 were included. The inclusion criteria were fetuses that underwent both ultrasound and MRI examinations of the brain. Exclusion criteria were pregnant women who had MRI contraindications or claustrophobia, who refused the MRI examination, and who had no ultrasound report or weekly gestational assessment available.The MRI examinations were performed on a 1.5 Tesla (1.5T) system (MAGNETOM Amira, Siemens Shenzhen Magnetic Resonance Ltd., China) with a 13-channel body coil. The sequences included T2-weighted half-Fourier single-shot turbo spin-echo (T2-HASTE), T2-weighted true fast imaging with steady-state precession (T2-TrueFISP), diffusion-weighted imaging (DWI), and T1-weighted imaging (T1WI). The acquisition parameters are shown in Table 1.
The fetuses were divided into six groups according to the CC abnormality type and the presence or not of additional intracranial malformations. These were isolated complete ACC (CACC), isolated partial ACC (PACC), isolated hypoplasia of the CC (HCC), and CACC, PACC, and HCC with other malformations. The ultrasound and MR images were independently reviewed by two sonologists and radiologists blinded to the cases, respectively. Inter-rater agreement was evaluated using the kappa consistency test. The prenatal diagnosis using US and MRI was compared with the postnatal findings or pathologic biopsies. The differences were analyzed using the chi-square test or Fisher’s exact test.
Results
Four hundred and eighty-two pregnant women with fetuses suspected of having CC dysplasia were included. After applying the inclusion and exclusion criteria, 375 fetuses were enrolled in the study. The study flowchart is shown in Figure 1.The inter-observer agreement between the two sonologists and radiologists was good for patient classifications. The Kappa values of the ultrasound were 0.789, 0.834, 0.911, 0.824, 0.902, and 0.795 for isolated CACC, PACC, HCC, and CACC, PACC, and HCC with additional malformations, respectively. The Kappa values of the MRI were 0.889, 0.945, 0.906, 0.921, 0.867, and 0.934 for isolated CACC, PACC, and HCC, and CACC, PACC, and HCC with additional malformations, respectively.
There were 173 fetuses diagnosed with isolated CACC, 39 with isolated PACC, 41 with isolated HCC, 45 with CACC and additional abnormalities, 29 with PACC and additional abnormalities, 11 with HCC and additional abnormalities, and 37 with no abnormalities,some cases were shown in Figure 2. Details regarding the additional central nervous system abnormalities are listed in Table 2. The results showed that for the additional abnormalities, the diagnostic accuracy of MRI (96.5%) was significantly higher than that of ultrasound (52.9%; p=0.000), particularly for cerebellar vermis dysplasia and Dandy-Walker syndrome (p=0.021 and p=0.000, respectively).
The diagnostic accuracies of US for isolated CACC, PACC, and HCC, and CACC, PACC, and HCC with additional malformations were 84.4%, 69.2%, 58.5%, 68.9%, 51.7%, and 45.5%, respectively (Table 3). The overall accuracy of ultrasound was 66.1% (248/375). The diagnostic accuracies of MRI for isolated CACC, PACC, and HCC, and CACC, PACC, and HCC with additional malformations were 100.0%, 87.2%, 90.2%, 93.3%, 86.2%, and 81.8%, respectively. The overall accuracy of MRI was 95.2% (357/375). The chi-square test showed that there was a significant difference in the total accuracy between MRI and ultrasound with p-value<0.0001, and the accuracy of MRI was significantly higher than ultrasound, with both p-values<0.0001.
Discussion
Our research showed that MRI is significantly better than ultrasound for the diagnosis of CC abnormalities, particularly in patients with isolated PACC and HCC, and PACC and HCC with additional abnormalities. We further found that the CACC groups had the largest proportion of fetuses among the six groups.Conclusions
In conclusion, fetal MRI can help to assess CC and additional associated abnormalities and enhance prognostic consultations.Acknowledgements
No acknowledgement found.References
1. Jeret JS, SD, Wisniewski K, Fisch C. Frequency of agenesis of the corpus callosum in the developmentally disabled population as determined by computerized tomography.Pediatr Neurosci. 1985-1986;12(2):101-3.
2. O.A. Glenn, AJB, Magnetic Resonance Imaging of the Fetal Brain and Spine: AnIncreasingly Important Tool in Prenatal Diagnosis, Part 1.AJNR Am J Neuroradiol. 2006:1604-11.
3.Glenn OA, BJ, Magnetic resonance imaging of the fetal brain and spine: an increasingly important tool in prenatal diagnosis: part 2.AJNR Am J Neuroradiol. 2006 1807-14.
4.Santirocco, M, C Rodo, T Illescas, et al. Accuracy of prenatal ultrasound in the diagnosis of corpus callosum anomalies.J Matern Fetal Neonatal Med. 2019 Apr 29:1-6. 2019.
5.Manevich-Mazor, M, A Weissmann-Brenner, O Bar Yosef, et al. Added Value of Fetal MRI in the Evaluation of Fetal Anomalies of the Corpus Callosum: A Retrospective Analysis of 78 Cases.Ultraschall Med. 2018; 39:513-525.
6. Pashaj, S, E Merz Detection of Fetal Corpus Callosum Abnormalities by Means of 3D Ultrasound.Ultraschall Med. 2016; 37:185-94.
7. Ruland, AM, C Berg, U Gembruch, et al. Prenatal Diagnosis of Anomalies of the Corpus Callosum over a 13-Year Period.Ultraschall Med. 2016; 37:598-603.
Figures
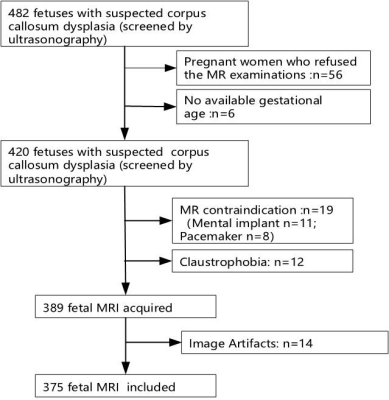
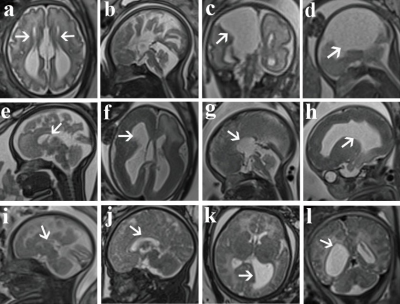
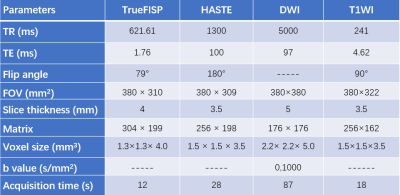
Table 1. Magnetic resonance protocol: Fetal CC parameters
TR, repetition time; TE, echo time; FOV, field of view; half-Fourier single-shot turbo spin-echo (HASTE), true fast imaging with steady-state precession (TrueFISP); diffusion-weighted imaging (DWI); and T1-weighted imaging (T1WI)
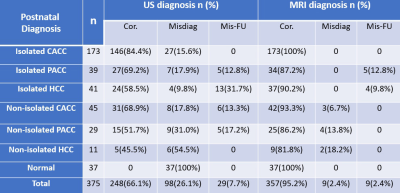
Table 3. Diagnosing fetal CC abnormalities in the postnatal, ultrasound (US), and magnetic resonance imaging (MRI) diagnostic groups
Cor., correct diagnosis; Misdiag, misdiagnosis; Mis-FU, missed diagnosis Isolated CACC, Isolated complete agenesis of the corpus callosum; Isolated PACC, Isolated partial agenesis of the corpus callosum; Isolated HCC, Isolated hypoplasia of the corpus callosum; Non-isolated CACC, CACC with other malformations; Non-isolated PACC: PACC with other malformations; Non-isolated HCC: HCC with other malformations.